PYQ Relevance:[UPSC 2024] In a crucial domain like the public healthcare system, the Indian State should play a vital role to contain the adverse impact of marketisation of the system. Suggest some measures through which the State can enhance the reach of public healthcare at the grassroots level. Linkage: The role of the state in the public healthcare system and asks for measures to enhance the reach of public healthcare, particularly at the grassroots level. The “medical oxygen access gap” is fundamentally a problem of the public healthcare system’s inability to reach everyone with this essential medicine. |
Mentor’s Comment: Recently, the oxygen shortage has been very serious in South Asia and East Asia-Pacific, where 78% and 74% of people do not have proper access to medical oxygen. Even though oxygen is essential for saving lives and became widely known during the COVID-19 pandemic, many low- and middle-income countries still face problems with its high cost, low supply, and poor access. Unlike medicines, there is no replacement for oxygen, which makes this a serious issue of fairness, basic rights, and survival. The WHO and The Lancet have suggested solutions, but progress has been slow. This is not just about fixing systems—it’s about saving lives, and action is urgently needed.
Today’s editorial talks about the problem of oxygen shortage in Southeast Asia. This topic is useful for GS Paper II (International Relations and Health Sector).
_
Let’s learn!
Why in the News?
Recently,’ The Lancet Global Health Commission has pointed out a serious and ongoing medical oxygen crisis, with 5 billion people around the world unable to get safe, good-quality, and affordable medical oxygen.
What challenges hinder global access to medical oxygen?
|
Why is oxygen demand high in South and East Asia?
- High Population Density: These regions have some of the world’s most densely populated countries, leading to higher disease burden and medical oxygen demand. Eg: India and China together account for over one-third of the global population, increasing strain on healthcare infrastructure during health crises like COVID-19.
- Prevalence of Respiratory Diseases: High rates of respiratory illnesses such as pneumonia, tuberculosis, and chronic obstructive pulmonary disease (COPD) elevate oxygen needs. Eg: According to WHO, India sees over 120,000 pneumonia-related child deaths annually, many requiring oxygen therapy.
- Inadequate Healthcare Infrastructure in Rural Areas: Many remote and underserved areas lack sufficient oxygen production, storage, and delivery systems. Eg: During the second COVID-19 wave in Nepal, rural hospitals reported severe oxygen shortages due to lack of concentrators and cylinders.
Where has WHO improved oxygen access through cooperation?
- Bhutan: WHO partnered with Nepal’s National Health Training Center to train biomedical engineers and technicians. Eg: This led to the installation of state-of-the-art PSA oxygen plants in Bhutan, ensuring sustainable operations and maintenance.
- Nepal: WHO supported capacity-building through regional training programs and technical support. Eg: Trained personnel strengthened Nepal’s oxygen infrastructure, especially during COVID-19.
- South-East Asia Region (broad cooperation): WHO facilitated intra-regional collaboration to boost oxygen capacity and resource sharing. Eg: Regional cooperation helped countries like Bangladesh and Sri Lanka improve oxygen planning and emergency response.
Who is responsible for strengthening oxygen ecosystems?
What has been done by the Indian government in Southeast Asia?
|
Way forward:
- Strengthen Local Infrastructure: Governments and partners must invest in decentralised oxygen production, solar-powered systems, and skilled workforce development to ensure reliable access, especially in rural and remote areas.
- Establish Robust Policies & Partnerships: Create strong regulatory frameworks and foster public-private-global collaborations to improve oxygen quality, supply chain efficiency, and emergency preparedness across regions.
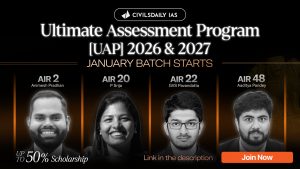
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024