Antibiotics Resistance
Antibiotic Pollution from the Manufacturing Process
From UPSC perspective, the following things are important :
Prelims level: Antibiotic Pollution
Why in the News?
The World Health Organization (WHO) released its first-ever global guidance on managing antibiotic pollution from manufacturing processes.
What is Antibiotic Pollution?
|
How does Antibiotic Pollution occur from the Manufacturing Process?
- Wastewater Discharge: Antibiotic plants release wastewater with residual antibiotics and active pharmaceutical ingredients (APIs) into local water bodies, contributing to drug-resistant bacteria.
- Improper Solid Waste Disposal: Unused antibiotics, raw materials, and by-products are often disposed of improperly, contaminating soil and groundwater.
- Inadequate Treatment: Many facilities lack effective systems to treat pharmaceutical waste, allowing antibiotics to enter the environment.
- Mass Balance Calculations: Inefficient systems or mismanagement can lead to unintentional antibiotic discharge during recycling and waste estimation.
- Leaks and Spills: Accidental leaks or spills during manufacturing, transportation, or storage introduce antibiotics into ecosystems.
- Runoff: Rainwater can carry antibiotics from waste into nearby rivers, lakes, or agricultural land, further contaminating the environment.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Are antibiotics over-prescribed in India?
From UPSC perspective, the following things are important :
Prelims level: H1 Rule
Mains level: Addressing AMR requires a holistic approach
Central Idea:
The National Centre for Disease Control (NCDC) conducted a study revealing that over half of the surveyed hospital patients in India were given antibiotics preventively rather than for treatment. This overuse of antibiotics poses a significant risk as India already faces a high burden of drug-resistant pathogens, contributing to antimicrobial resistance (AMR). Experts Sumit Ray and Abdul Ghafur discuss the causes, consequences, and potential solutions to this issue, emphasizing the need for judicious antibiotic use and addressing systemic challenges.
Key Highlights:
- Antimicrobial Resistance (AMR): AMR refers to microorganisms becoming resistant to antibiotics. India is grappling with high levels of drug-resistant bacteria, impacting patient outcomes negatively.
- Factors Leading to AMR: Inappropriate antibiotic use, lack of rapid diagnostics, insufficient training, inadequate monitoring, and pharmaceutical industry incentives contribute to the rise of AMR.
- NCDC Survey Findings: The survey showed that 55% of patients received antibiotics as a preventive measure, indicating a potential over-prescription issue.
- Root Causes of Over-Prescription: Overcrowded hospitals, limited access to rapid diagnostics, and economic factors drive doctors to opt for antibiotics as a quicker and cheaper alternative.
- Immediate Threat: The immediate danger is evident in the survey’s findings, with a significant percentage of patients exhibiting resistance to various generations of antibiotics, leading to poor health outcomes.
- AMR as a Complex Challenge: AMR is not solely a medical issue but a complex challenge involving socio-economic, political, and infrastructural factors.
Key Challenges:
- Over-Prescription: Doctors tend to prescribe antibiotics unnecessarily due to factors like overcrowded hospitals, limited time for examinations, and inadequate diagnostic facilities.
- Lack of Rapid Diagnostics: The absence of quick and affordable diagnostic tools contributes to the inappropriate use of antibiotics.
- Systemic Issues: Weak governance, inadequate sanitation, poverty, and limited access to clean water are interconnected factors contributing to AMR.
- Implementation Gap: Existing guidelines for antibiotic use exist, but there is a gap in their implementation, leading to over-prescription.
- Incentivization in Pharma Industry: The pharmaceutical industry’s encouragement of certain prescribing practices exacerbates the problem.
Key Terms/Phrases:
- Antimicrobial Resistance (AMR): Microorganisms becoming resistant to antibiotics.
- Over-the-Counter Antibiotics: Antibiotics available without a prescription.
- H1 Rule: Regulation prohibiting certain antibiotics without a prescription.
- Colistin: A potent antibiotic, banned for growth promotion in poultry farming.
- Third/Fourth-Generation Antibiotics: Antibiotics of advanced generations, facing resistance in bacterial strains.
Key Quotes:
- “I treat infections in cancer patients, who are the most immuno-compromised patients you can come across. Patients are losing their lives because of AMR.” – Abdul Ghafur
- “What is essential is the linking of labs to all levels of clinical setups and the fast transmission of infection-related data between the lab and the clinician.” – Sumit Ray
Key Examples and References:
- National Centre for Disease Control (NCDC) survey on antibiotic use in Indian hospitals.
- Indian government’s 2019 ban on colistin use in poultry farming.
Critical Analysis:
- Overcrowded hospitals and limited diagnostic access drive over-prescription.
- Addressing AMR requires a holistic approach, considering socio-economic factors.
Way Forward:
- Restrict access to reserve antibiotics to reduce resistance.
- Improve public health systems, delivery, and sanitation to curb AMR.
- Enforce existing laws, such as the ban on over-the-counter antibiotic sales.
In conclusion, addressing the overuse of antibiotics in India requires a multifaceted approach, involving improvements in healthcare infrastructure, diagnostic capabilities, and enforcement of regulations. The goal is to mitigate the immediate threat of AMR and ensure the judicious use of antibiotics for effective treatment.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
India’s alarming ‘fixed dose combination’ problem
From UPSC perspective, the following things are important :
Prelims level: Antimicrobial Resistance (AMR)
Mains level: safety and efficacy of pharmaceutical products
Central idea
The study reveals a startling prevalence of unapproved and banned Fixed Dose Combinations (FDCs) of antibiotics in India, posing risks of antimicrobial resistance. The pharmaceutical industry’s exploitation of FDCs to evade regulations, coupled with regulatory inefficiencies, calls for urgent interventions to safeguard public health
Key Highlights:
- Alarming Prevalence: In 2020, 60.5% of antibiotics in India were unapproved FDCs, with an additional 9.9% banned, raising concerns about antimicrobial resistance.
- Patient Compliance vs. Risks: FDCs, aimed at improving patient adherence, pose risks due to potential interactions between combined drugs, necessitating a stringent approval process.
- Pharmaceutical Industry’s Strategy: Exploitation of FDCs allows the industry to evade drug price regulations, contributing to the proliferation of irrational combinations.
Key Challenges:
- Regulatory Framework Inefficiency: Continued sale of unapproved FDCs highlights regulatory inefficiency, allowing non-compliance despite existing legal provisions.
- Reactive Regulatory Measures: Reliance on Section 26A orders reveals a reactive rather than proactive regulatory approach, indicating systemic challenges.
Key Terms:
- Fixed Dose Combination (FDC): Combinations of multiple drugs in a single dosage form, potentially affecting drug interactions and therapeutic efficacy.
- Antimicrobial Resistance (AMR): The ability of microorganisms to resist the effects of medications, posing a global health threat.
Key Phrases:
- Pharmaceutical Industry’s Exploitation: The strategic use of FDCs to avoid regulatory scrutiny undermines the integrity of drug pricing and quality.
- Ineffectiveness of Regulatory Measures: Despite legal provisions, the regulatory system relies on reactive prohibitions rather than proactive prevention.
Key Quotes:
- “Unapproved FDCs may contribute to the AMR problem in India.”
- “The pharmaceutical industry gets to provide its own standards for government testing of FDCs.”
Key Statements:
- Extent of the Issue: The study underscores the alarming prevalence of unapproved and banned FDCs in India, emphasizing the urgent need for regulatory intervention.
- Industry Motives: The article critically examines the pharmaceutical industry’s profit-driven motives, exposing the imbalance between pseudo-innovation for profit and genuine drug development.
- Regulatory Challenges: Scrutiny of regulatory challenges and legal inconsistencies indicates a systemic failure in ensuring the safety and efficacy of pharmaceutical products.
Key Examples and References:
- Academic Study: Reference to the academic study published in the Journal of Pharmaceutical Policy and Practice (2023) highlighting the extent of unapproved FDCs.
- Historical Context: Tracing the issue back to 1978 and subsequent regulatory amendments provides context to the ongoing challenges.
Critical Analysis:
- Industry Practices: The article critically examines the pharmaceutical industry’s motives, highlighting the imbalance between pseudo-innovation for profit and genuine drug development.
- Regulatory Challenges: Scrutiny of regulatory challenges and legal inconsistencies indicates a systemic failure in ensuring the safety and efficacy of pharmaceutical products.
Way Forward:
- Urgent Regulatory Actions: Emphasizes the need for regulatory actions to address the menace of unapproved and banned FDCs, preventing potential contributions to antimicrobial resistance.
- Proactive Regulatory Framework: Calls for a proactive regulatory framework that prioritizes public health over industry interests and plugs existing legal loopholes.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Don’t ignore the threat of antimicrobial resistance
Central idea
The article highlights challenges in combating Antimicrobial Resistance (AMR), citing an implementation gap in National Action Plans. It calls for global collaboration, emphasizing regional plans, international funding, and patent reforms. Key data underscores the urgency, especially in G20 nations, where coordinated efforts are crucial to address the significant toll of AMR-related deaths.
What is antimicrobial resistance?
Antimicrobial Resistance (AMR) is when germs like bacteria and viruses become strong and don’t respond to medicines, making the medicines not work well. This is a big problem because it makes it hard to treat infections, and the resistant germs can spread. We need to work together to make sure our medicines keep working against these germs.
Key Highlights:
- Delhi Declaration Commitments: The G20, including India, pledged to strengthen global health systems, implement the One Health approach, and prioritize tackling Antimicrobial Resistance (AMR) through research and development (R&D).
- AMR’s Global Impact: A Lancet report revealed that AMR caused 4.95 million deaths globally, comparable to HIV and malaria. Sub-Saharan Africa and South Asia faced the highest death rates.
- G20’s Significance: G20 countries, housing over 60% of the world’s population, address AMR’s threat. Africa, now part of the coalition, adds complexity due to lower investments in healthcare infrastructure.
Challenges and Concerns:
- Implementation Gap: Despite comprehensive National Action Plans (NAPs), the efficacy varies, hindering the global effort against AMR.
- Global Disparities: Low and middle-income countries, especially in Africa, face challenges in dealing with AMR due to limited healthcare infrastructure investments.
Analysis:
- Global Collaboration Needed: The success of the Delhi Declaration requires global and local efforts. Prioritizing regional AMR action plans, international funding for R&D, and patent reforms are crucial.
- Local-Level Action: Effective implementation of NAPs, strengthening surveillance, and promoting responsible antibiotic use are imperative. India’s existing initiatives like Free Diagnostic Services and Kayakalp can play a pivotal role.
Key Data and Facts:
- AMR’s Toll: Lancet’s 2021 report associates 1.27 million deaths directly with bacterial AMR, with Sub-Saharan Africa and South Asia facing the highest death rates.
- G20’s Population Impact: G20 countries house over 60% of the world’s population, making their commitment crucial in tackling AMR globally.
Way Forward:
- Regional Action Plans: G20 countries should collaborate with developing nations to create regional AMR action plans, enhancing global coordination.
- International Funding Mechanism: Advocating for an international funding mechanism focusing on AMR R&D is vital to address global disparities.
- Patent Reforms: G20 nations should consider promoting patent reforms to foster innovation and ensure affordability in new antibiotics, learning from models like the Medicines Patent Pool.
- Local-Level Prioritization: Countries need to prioritize NAP implementation, expand monitoring networks, and promote responsible behavior to combat AMR effectively.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
The challenge of Antimicrobial Resistance (AMR), and how to confront it effectively
From UPSC perspective, the following things are important :
Prelims level: Antimicrobial Resistance and various diseases caused by pathogens
Mains level: Rising Antimicrobial Resistance, concerns and measures
What’s the news?
- Antimicrobial Resistance (AMR) is today reckoned among the most ominous threats confronting Global Public Health. There is an urgent need for a collective and comprehensive approach to address the global threat of AMR and the role of various stakeholders in prevention, control, and surveillance efforts is crucial.
Definition
- Antimicrobial resistance, means that certain drugs that were once effective in treating infections caused by bacteria, viruses, fungi, or parasites no longer work because the pathogens have become resistant to them.
- In simpler terms, it is when the germs that make us sick become “immune” to the medicines we use to treat them.
Prevalence of AMR
- According to recent estimates, in 2019, 1.27 million deaths were directly attributed to drug-resistant infections globally. By 2050, up to 10 million deaths could occur annually.
- If unchecked, AMR could shave US$ 3.4 trillion off GDP annually and push 24 million more people into extreme poverty in the next decade.
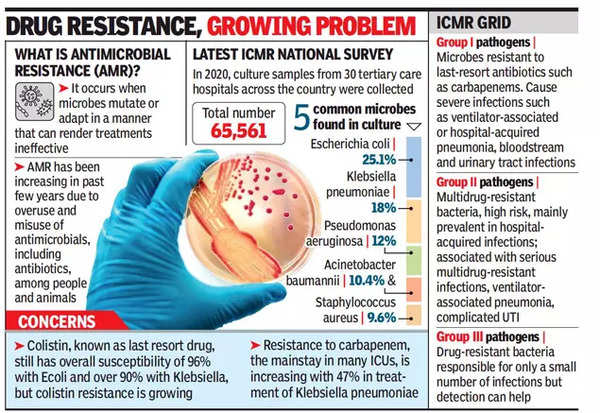
- A 2022 study by the Indian Council of Medical Research (ICMR) revealed that resistance to broad-spectrum antimicrobials increases by 5% to 10% every year.
AMR: A concern for global public health
- Rising Resistance: The infections caused by the pathogens including bacteria, viruses, fungi, and parasites, are increasingly developing resistance to antimicrobial drugs which is becoming more challenging to treat effectively.
- Treatment Failures: AMR can lead to treatment failures, as commonly used antibiotics, antivirals, antifungals, and antiparasitic drugs may no longer be effective against resistant strains.
- Healthcare Impact: AMR increases the complexity and cost of treatment, prolongs hospital stays, and requires the use of stronger and more expensive drugs. Healthcare-associated infections caused by drug-resistant pathogens are a particular concern.
- Limited Drug Pipeline: The development of new antimicrobial drugs has slowed down in recent years. There is a lack of new effective treatments to replace those that are losing effectiveness due to resistance.
- Global Spread: AMR is a global issue that knows no boundaries. Resistant pathogens can spread between countries through travel and trade, and international cooperation is crucial.
Current Scenario of AMR prevention and National Action Plans
- Over the last ten years, the prevention, control, and response to AMR has been a high priority for most national governments, international organisations (such as the WHO, FAO, OIE), healthcare communities, and civil society, etc.
- The WHO’s global action plan (GAP) was adopted by member nations in 2015.
- National action plans have been prepared by many countries.
- India’s NAP was approved in 2017. It is understood that NAP 2.0 is now envisaged.
- In 2015, the WHO launched the Global Action Plan (GAP) on AMR, which provides a strategic framework for countries to develop their national action plans.
- AMR is an important priority in the G20 health agenda under India’s presidency.
India’s national action plan to combat AMR
- Coordinated Action: India’s NAP emphasizes coordinated action by the government and non-government sectors. It involves a whole of government approach, involving sectors like Health, Animal Husbandry, Fisheries, Agriculture, Dairy, Pharmaceuticals, and Biotechnology.
- Advocacy and Awareness: The plan focuses on advocacy and awareness-building activities to educate healthcare professionals, policymakers, and the general public about responsible antimicrobial use and AMR prevention.
- Community Involvement: India’s NAP It emphasizes engaging and empowering communities to promote responsible use of antimicrobials.
- Infection Prevention and Control: The NAP emphasizes infection prevention and control measures to reduce the spread of AMR. This includes promoting appropriate hygiene practices and implementing infection control protocols in healthcare settings.
- National AMR Surveillance Network (NARS Net): India has established the National AMR Surveillance Network to monitor and track the prevalence and patterns of AMR across the country. This surveillance system helps in generating data for evidence-based interventions.
- Research and International Collaboration: India’s NAP emphasizes the importance of research on AMR and encourages international collaboration in this field.
Need for a concerted, combined effort to address AMR
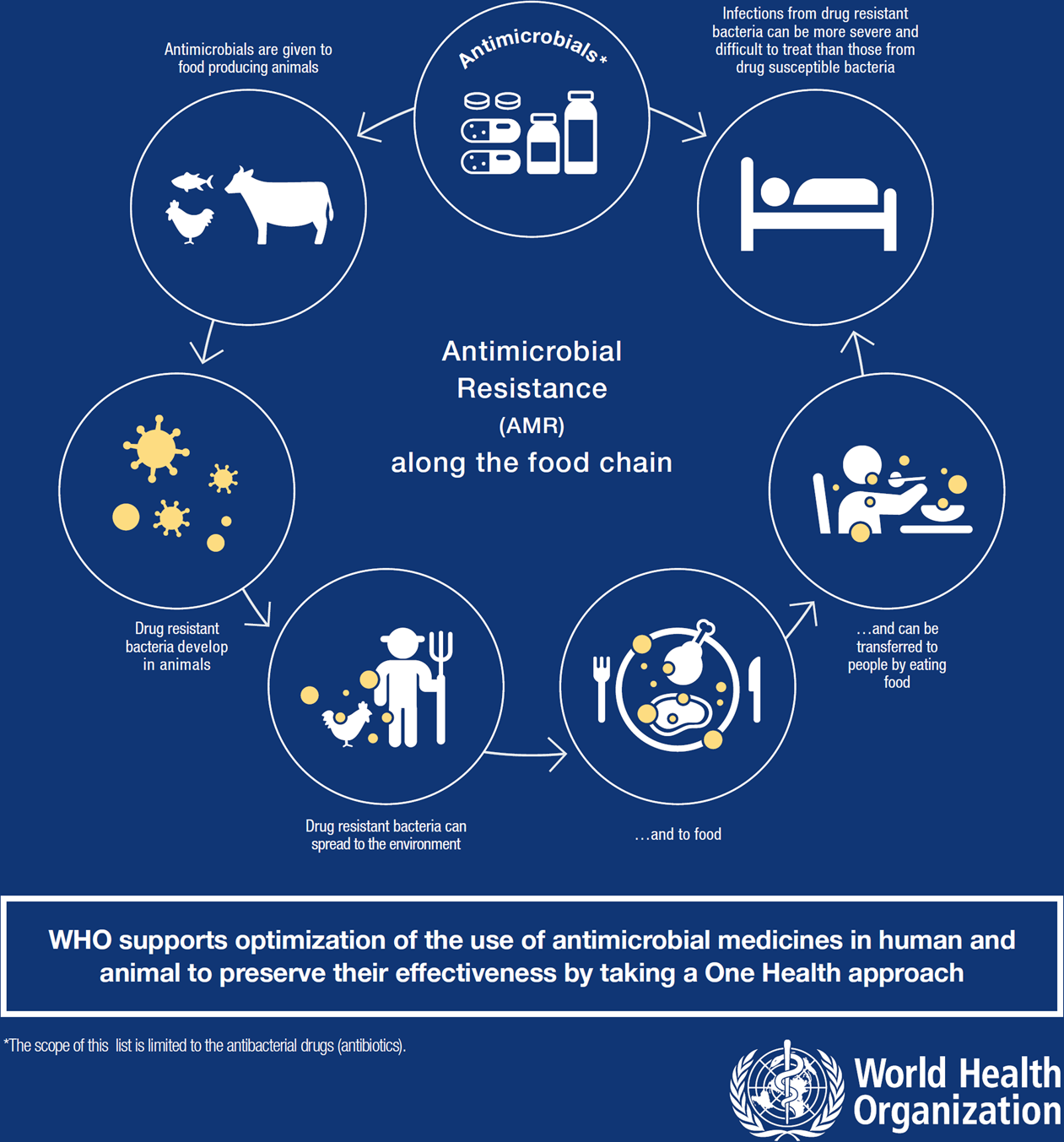
- One Health Approach: AMR requires a One Health approach, recognizing the interconnectedness of human health, animal health, and the environment. Collaborative efforts among human and veterinary healthcare sectors, agriculture, environmental agencies, and other stakeholders are necessary to tackle AMR comprehensively.
- Stakeholder Involvement: The sectors responsible for food, drinking water, and the environment should share equal ownership in addressing AMR. Regulating antibiotic access and usage in non-human consumption sectors, such as animal husbandry and poultry, is vital.
- State and Local Engagement: Implementation of infection control measures, regulation of pharmacies, treatment of sewage and pharmaceutical effluents, and AMR surveillance are primarily implemented at the state level.
- Environmental Considerations: Efforts should be made to prevent the contamination of the environment by untreated wastewater and effluents, including those from antibiotics manufacturing units and healthcare facilities. Effective sanitation and waste treatment infrastructure are necessary to combat AMR.
- Surveillance and Data: Robust surveillance systems are crucial to monitor AMR patterns and trends. Collecting and analyzing data on antimicrobial use, resistance prevalence, and treatment outcomes helps inform evidence-based interventions.
What’s more?
- Parallel efforts on a war footing are needed for the discovery and commercialisation of new antibiotics and new antimicrobials. Such efforts must be incentivised.
- Social media and its numerous platforms have captured the imagination of people around the world. The influence of social media on our mind and behaviour cannot be denied. We
- Considering its influence on our mind and behaviour, social media and its numerous platforms must be leveraged to spread the message of AMR.
- Objective should be to inculcate community realisation for rational and correct use of antimicrobials.
Conclusion
- Addressing the global challenge of AMR demands a collective and coordinated effort involving various stakeholders. Embracing novel solutions, such as new diagnostics, alternative treatments, and technology-driven interventions, is essential. By embracing these measures, we can protect public health, alleviate economic burdens, and secure a healthier future for all.
Also read:
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Antimicrobial Resistance (AMR): An Invisible Pandemic
From UPSC perspective, the following things are important :
Prelims level: AMR
Mains level: AMR challenges and Government measures
Central Idea
- While the world is emerging from the acute phase of the COVID-19 pandemic, the very harmful but invisible pandemic of Antimicrobial Resistance (AMR) is unfortunately here to stay. Most countries understood in 2020 the clear and present danger of COVID-19, forcing governments, including India’s, to respond with speed and accuracy. The rapidly rising AMR rates also need an accelerated, multi-sectoral, global and national response.
Crack Prelims 2023! Talk to our Rankers
What is Antimicrobial Resistance (AMR)?
- Antimicrobial resistance (AMR) is a natural phenomenon that occurs when microorganisms such as bacteria, viruses, fungi, and parasites evolve to become resistant to antimicrobial drugs such as antibiotics, antivirals, antifungals, and antiparasitics that were previously effective in treating infections caused by those microorganisms.
The Threat of Antimicrobial Resistance
- Human deaths: In 2019, AMR caused approximately 4.95 million human deaths worldwide, highlighting the urgency of addressing this issue.
- Report by OECD: A 2018 report by the Organisation for Economic Co-operation and Development warned that the world could experience a significant rise in resistance to second and third-line antibiotics by 2030.
- Resistance increases by 5% to 10% every year: A 2022 study by the Indian Council of Medical Research (ICMR) revealed that resistance to broad-spectrum antimicrobials increases by 5% to 10% every year.
- High rate of resistance found in commonly used drugs: The Indian Network for Surveillance of Antimicrobial Resistance (INSAR) also found a high rate of resistance to commonly used drugs such as ciprofloxacin, gentamicin, co-trimoxazole, erythromycin, and clindamycin, underscoring the importance of taking steps to combat AMR.
- High levels of resistance: WHO has increasingly expressed concern about the dangerously high levels of antibiotic resistance among patients across countries.
- For example: Ciprofloxacin, an antibiotic commonly used to treat urinary tract infections. According to WHO, resistance to ciprofloxacin varied from 8.4% to 92.9% for Escherichia coli (E. coli) and from 4.1% to 79.4% for Klebsiella pneumoniae (a bacteria that can cause life-threatening infections such as pneumonia and intensive care unit- related infections). The global epidemic of TB has been severely impacted by multidrug resistance patients have less than a 60% chance of recovery.
- Adds burden to communicable disease: AMR adds to the burden of communicable diseases and strains the health systems of a country, making it even more challenging to address health crises.
What is Muscat conference is about?
- Ministerial Conference on AMR: Third Global High-Level Ministerial Conference on Antimicrobial Resistance (November 24-25, 2022) held in Muscat where over 30 countries adopted the Muscat Ministerial Manifesto on AMR.
- The conference focused on three health targets:
- Reduce the total amount of antimicrobials used in the agri-food system at least by 30-50% by 2030;
- Eliminate use in animals and food production of antimicrobials that are medically important for human health;
- Ensure that by 2030 at least 60% of overall antibiotic consumption in humans is from the WHO Access group of antibiotics.
- Muscat Manifesto:
- Need to accelerate One Health action: The manifesto recognised the need to accelerate political commitments in the implementation of One Health action for controlling the spread of AMR.
- Need to address the overall impact of AMR: It also recognised the need to address the impact of AMR not only on humans but also on animals, and in areas of environmental health, food security and economic growth and development.
Government efforts so far
- The National Action Plan on Antimicrobial Resistance (2017-21): The National Action Plan on AMR emphasised the effectiveness of the government’s initiatives for hand hygiene and sanitation programmes such as Swachh Bharat Abhiyan, Kayakalp and Swachh Swasth Sarvatra.
- Increasing community awareness: The government has also attempted to increase community awareness about healthier and better food production practices, especially in the animal food industry.
- Specific guidelines regarding use and limiting use of antibiotics: The National Health Policy 2017 also offered specific guidelines regarding use of antibiotics, limiting the use of antibiotics as over-the-counter medications and banning or restricting the use of antibiotics for growth promotion in livestock.
- Called for scrutiny of antibiotic prescriptions: It also called for scrutiny of prescriptions to assess antibiotic usage in hospitals and among doctors.
Examples of Limiting AMR worldwide
- Less use of Antimicrobials less likely resistance: Scientific evidence suggests that the less antimicrobials are used, it is less likely that there will be an emergence of drug resistance.
- Netherlands and Thailand: Countries such as the Netherlands and Thailand have decreased their usage by almost 50%.
- China: In China, the consumption of antibiotics in the agricultural sector has fallen substantially.
Way ahead: India’s role
- India committed to strengthen surveillance: India has committed to strengthening surveillance and promoting research on newer drugs.
- GLASS: It also plans to strengthen private sector engagement and the reporting of data to the WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) and other standardised systems.
Conclusion
- The various G-20 health summits spread through 2023 offer an opportunity for India to ensure that all aspects of AMR are addressed and countries commit to progress. As the current G-20 president, and as a country vulnerable to this silent pandemic, India’s role is critical in ensuring that AMR remains high on the global public health agenda.
Mains question
Q. In the backdrop of recently held Muscat Conference on AMR highlight the threats posed by AMR and Discuss India’s efforts in combating the silent pandemic.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Antimicrobial resistance (AMR): The silent health catastrophe
From UPSC perspective, the following things are important :
Prelims level: Antimicrobial resistance (AMR)
Mains level: Antimicrobial resistance, challenges and preventive measures
Context
- Antimicrobial resistance (AMR), often also called antibiotic resistance, is a global health challenge and a looming public health crisis. The WHO has declared it as one of the top 10 health threats facing humanity.
Crack Prelims 2023! Talk to our Rankers
What is antimicrobial resistance (AMR)?
- AMR is the ability of a microorganism (like bacteria, viruses, and some parasites) to stop and survive exposure to an antimicrobial (such as antibiotics, antivirals and antimalarials) from working against it. As a result, standard treatments become ineffective, infections persist and may spread to others.
How AMR occurs?
- Improper use of antimicrobials: Antimicrobials, chemicals or molecules that kill harmful bugs, are the backbone of modern medicine. Improperly used antimicrobials create selective pressure on bugs.
- Resilient bugs survive the exposure to antimicrobials: The bugs most vulnerable to the drugs die quickly, while the most resilient ones survive, replicate and become superbugs. AMR occurs when superbugs develop and antimicrobials stop working.
- For example: Microorganisms (bugs) are everywhere with some being helpful like the yoghurt-making lactobacillus and some being harmful like the typhoid-causing salmonella.
What are superbugs?
- Microorganisms that become resistant to most antimicrobials are often referred to as superbugs.
- Superbugs makes medical procedures such as organ transplantation, cancer chemotherapy, and other major surgeries very risky.
Interesting fact
- Research has shown that the use of certain types of antimicrobials in animal feed can lead to the development of antimicrobial-resistant bacteria in food-producing animals.
- These resistant bacteria can then be transmitted to humans through the food supply, leading to the spread of AMR.
Prescription to reduce and potentially reverse AMR
- The first prescription is prevention: Disease prevention and wellness are key to public health and thus preventing infections whenever and wherever possible is equivalent to averting resistance. We need to spearhead sanitation drives, ensure a clean water supply and support hospital-driven infection-control programmes.
- Judicious prescription of antimicrobials: Reducing AMR also requires prescribing antimicrobials judiciously and only when they are absolutely needed.
- Effective coordination and management: There is also a need for more cohesion within management strategies. Coordination across the animal industry and environmental sectors to prevent the unnecessary use of antibiotics in farms these nurtures drug-resistant organisms in our food supply is necessary.
- Robust surveillance systems to detect resistant pathogens of all kinds: Other prescription closely connected with prevention is the development of robust surveillance systems that allow us to detect resistant pathogens of all kinds in the environment and hospitals that would eventually allow containment.
- Heavy investment in research and development: There is an urgent need for a strong pipeline of new antibiotics; an essential component in restoring the balance and ensuring that we have new tools in the fight against AMR. Bringing a new antibiotic from basic research through clinical trials takes more than a decade and requires upward of $1 billion. So there is need to invest heavily in research and development through both government and private funding.
- New financial incentives to make it profitable keeping in mind the social value: Profits on these drugs are negligible. Hence, there is need to formulate new types of financial incentives to measure return on investment and measure profitability by the social value of the antibiotic, breaking the conventional link between sales and profits.
- Bringing in the collective moral vision: Last but not least, we need to bring a collective moral vision to AMR and start thinking of antibiotic/antimicrobial drugs as limited resources that should be available to all.
Conclusion
- Although seemingly distant and abstract, AMR is in the air and potentially catastrophic for those burdened by it. The success of modern medicine, women’s health, infectious diseases, surgery and cancer would be at increased risk for lack of working antimicrobials. The cost of AMR to the economy is significant and it is critical to develop policies and implement them through a holistic One Health approach.
Mains question
Q. What is Antimicrobial Resistance (AMR)? Given that AMR is an impending health disaster, discuss what measures can be taken to reduce AMR?
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Limiting the Anti-Biotic Pollution and Anti-microbial resistance (AMR)
From UPSC perspective, the following things are important :
Prelims level: Anti-microbial resistance (AMR)
Mains level: Anti-biotic Pollution, Anti-microbial resistance (AMR) and its impact
Context
- Almost half, or 43 per cent, of the world’s rivers are contaminated with active pharmaceutical ingredients in concentrations that can have disastrous ramifications on health. The industry must prioritize wastewater management and process controls to limit antibiotic pollution and Anti-microbial resistance (AMR). 18-22 November is observed as World Antimicrobial awareness week.
What is Anti-microbial resistance (AMR)?
- Antimicrobial resistance (AMR or AR) is the ability of a microbe to resist the effects of medication that once could successfully treat the microbe
- Antibiotic resistance occurs naturally, but misuse of antibiotics in humans and animals is accelerating the process.
- A growing number of infections – such as pneumonia, tuberculosis, gonorrhoea, and salmonellosis – are becoming harder to treat as the antibiotics used to treat them become less effective.
- It leads to higher medical costs, prolonged hospital stays, and increased mortality.

Importance of Pharma Industry
- Important sector of economy: The recently adopted Glasgow Climate Pact has called upon countries to facilitate the adoption of greener technologies to phase out the use of fossil fuels. The development and deployment of such technologies is also critical for the pharmaceutical sector that has formed the backbone of the growth of many economies including India.
- Improving the health outcomes: The Pharma sector plays a fundamental role in improving health outcomes through the invention of life-saving products.
- 20% of global supply of medication: Pivoting to sustainable waste management and process-control practices assumes acute significance in the Indian context. India already accounts for 20 per cent of the global supply of medication, making it the largest supplier of generic medicines worldwide.
Anti-biotic Pollution and Anti-microbial resistance (AMR)
- Pharmaceutical pollution in the country: Recently, widescale pharmaceutical pollution has been reported across the country, particularly in pharmaceutical hubs like Himachal Pradesh, Andhra Pradesh, and Telangana.
- Untreated waste release into rivers: The release of untreated effluents into the soil and water bodies add to the pollution of the environment during the manufacturing of various pharmaceuticals, including antibiotics. Further, untreated antibiotic residues also accelerate the build-up of antimicrobial resistance (AMR).
- High emission intensity: Pharma sectors emission intensity is 55 per cent more than the automotive sector.
- AMR is public health threat: AMR is often dubbed as one of the top 10 public health threats facing humanity. It occurs when disease-causing pathogens develop a resistance against the pharmaceuticals that could have neutralized them. In 2019, AMR accounted for more than half a million deaths in the European region and about five million globally.
- Accumulation of AMR in ecosystem: The build-up of AMR can happen due to several factors across the human, animal, and environmental ecosystems.
Government policies to prevent Anti-biotic pollution in India
- National Action Plan on AMR (NAP-AMR): India’s production capacity is all set to expand further with the government’s recent impetus on the domestic production of pharmaceuticals. Against this background, the country’s National Action Plan on AMR (NAP-AMR) called for limiting pharmaceutical pollution.
- Surveillance of residues discharged: Strategic Pillars 2 and 3 under the NAP-AMR focused on developing frameworks for the surveillance of residues discharged in the environment and developing a plan to reduce the environmental impact on AMR, respectively. However, this policy impetus is yet to translate into on-ground implementation.
- Benefits to manufacturers with greener practices: The government can take a cue from countries like the United Kingdom, Norway, Sweden and Germany, among others, which have policies in place that provide benefits to manufacturers with greener practices.
How pharmaceutical industry can improve its waste management?
- Use of innovative technologies: Adopting innovative technology and self-regulation can help the industry reduce its carbon footprint and minimize its environmental impact.
- State-of-art API technology: Centrient Pharmaceuticals Netherlands BV’s plant at Toansa, Punjab, where the adoption of state-of-art API technology led to a 60-62 per cent reduction in the plant’s carbon footprint.
- Regulating the discharge: The AMR Industry Alliance (AMRIA) has developed the Predicted No-Effect Concentrations (PNEC) criteria further to facilitate the industry in regulating its discharge of effluents.
- Strict compliance of guidelines: The compliance to PNEC value for Centrist’s oral API product line and supply chain has helped the company reduce the environmental impact of manufacturing.
Conclusion
- The containment of AMR in India is crucial for realizing several policy goals, including the United Nations Sustainable Development Goals. While collective action is needed from various stakeholders, the domestic pharmaceutical industry should also take the lead, especially in limiting antibiotic pollution.
Mains Question
Q. Explain the linkages between Anti-biotic pollution and anti-microbial resistance (AMR). How government and pharma industry join the hands to reduce the anti-biotic pollution?
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Anti-microbial resistance needs urgent attention
From UPSC perspective, the following things are important :
Prelims level: National Action Plan for AMR
Mains level: Paper 2- Dealing with the challenge of anti-microbial resistance
Context
Ever since the pandemic struck, concerns have been raised about the improper use of antimicrobials amongst Covid-19 patients.
Concern over anti-microbial resistance
- The “Global burden of bacterial antimicrobial resistance in 204 countries and territories in 2019 (GRAM)” report, released last month, 4.95 million people died from drug-resistant bacterial infections in 2019, with 3,89,000 deaths in South Asia alone.
- AMR directly caused at least 1.27 million of those deaths.
- Lower respiratory infections accounted for more than 1.5 million deaths associated with resistance in 2019, making it the most burdensome infectious syndrome.
- Amongst pathogens, E coli was responsible for the most deaths in 2019, followed by K pneumoniae, S aureus, A baumannii, S pneumoniae, and M tuberculosis.
Concern for India
- As per the yearly trends reported by the Indian Council of Medical Research since 2015, India reports a high level of resistance in all these pathogens, especially E coli and K pneumoniae.
- Only a fraction of the Indian data, available through the WHO-GLASS portal, has been included in the GRAM report.
- India has been reporting high levels of resistance to fluoroquinolones, cephalosporins and carbapenems across the Gram-negative pathogens that cause almost 70 per cent of infections in communities and hospitals.
- Therefore, the Indian data on the AMR burden may not look very different from the estimates published in the report.
- Now that we know that AMR’s burden surpasses that of TB and HIV, a sense of urgency in containing such resistance is called for.
- With no new drugs in the pipeline for drug-resistant infections, time is running out for patients.
Addressing AMR through a multipronged and multisectoral approach
- Use existing antimicrobials judiciously: The urgency to develop new drugs should not discourage us from instituting measures to use the existing antimicrobials judiciously.
- Improved infection control in communities and hospitals, availability and utilisation of quality diagnostics and laboratories and educating people about antimicrobials have proved effective in reducing antimicrobial pressure — a precursor to resistance.
- The National Action Plan for AMR, approved in 2017, completes its official duration this year. The progress under the plan has been far from satisfactory.
- There is enough evidence that interventions like infection control, improved diagnosis and antimicrobial stewardship are effective in the containment of AMR.
Conclusion
The GRAM report has underlined that postponing action could prove costly.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Antimicrobial resistance
From UPSC perspective, the following things are important :
Prelims level: Factors responsible for anti-microbial resistance
Mains level: Paper 2-Threats posed by anti-microbial resistance
The article highlights the challenges posed by anti-microbial resistance (AMR) and suggests ways to deal with it.
Understanding the severity of challenges posed by AMR
- Antimicrobial resistance (AMR) is the phenomenon by which bacteria and fungi evolve and become resistant to presently available medical treatment.
- AMR represents an existential threat to modern medicine.
- Without functional antimicrobials to treat bacterial and fungal infections, even the most common surgical procedures, as well as cancer chemotherapy, will become fraught with risk from untreatable infections.
- Neonatal and maternal mortality will increase.
How AMR will affect low and middle-income countries
- All these effects will be felt globally, but the scenario in the low- and middle-income countries (LMICs) of Asia and Africa is even more serious.
- LMICs have significantly driven down mortality using cheap and easily available antimicrobials.
- In the absence of new therapies, health systems in these countries are at severe risk of being overrun by untreatable infectious diseases.
Factors contributing to AMR
- Drug resistance in microbes emerges for several reasons.
- These include the misuse of antimicrobials in medicine, inappropriate use in agriculture, and contamination around pharmaceutical manufacturing sites where untreated waste releases large amounts of active antimicrobials into the environment.
Stagnant antibiotics discovery
- The Challenge of AMR is compounded by fact that no new classes of antibiotics have made it to the market in the last three decades.
- This has happened on account of inadequate incentives for their development and production.
- A recent report from the non-profit PEW Trusts found that over 95% of antibiotics in development today are from small companies, 75% of which have no products currently in the market.
- Major pharmaceutical companies have largely abandoned innovation in this space.
Measures to deal with the challenge of AMR
- In addition to developing new antimicrobials, infection-control measures can reduce antibiotic use.
- A mix of incentives and sanctions would encourage appropriate clinical use.
- To track the spread of resistance in microbes, surveillance measures to identify these organisms need to expand beyond hospitals and encompass livestock, wastewater and farm run-offs.
- Finally, since microbes will inevitably continue to evolve and become resistant even to new antimicrobials, we need sustained investments and global coordination to detect and combat new resistant strains on an ongoing basis.
Way forward
- A multi-sectoral $1 billion AMR Action Fund was launched in 2020 to support the development of new antibiotics.
- The U.K. is trialling a subscription-based model for paying for new antimicrobials towards ensuring their commercial viability.
- Other initiatives focused on the appropriate use of antibiotics include Peru’s efforts on patient education to reduce unnecessary antibiotic prescriptions.
- Australian regulatory reforms to influence prescriber behaviour, and initiatives to increase the use of point-of-care diagnostics, such as the EU-supported VALUE-Dx programme.
- Denmark’s reforms to prevent the use of antibiotics in livestock have led to a significant reduction in the prevalence of resistant microbes in animals and improved the efficiency of farming.
- Finally, given the critical role of manufacturing and environmental contamination in spreading AMR there is a need to curb the amount of active antibiotics released in pharmaceutical waste.
- Regulating clinician prescription of antimicrobials alone would do little in settings where patient demand is high and antimicrobials are freely available over-the-counter in practice, as is the case in many LMICs.
- Efforts to control prescription through provider incentives should be accompanied by efforts to educate consumers to reduce inappropriate demand, issue standard treatment guidelines.
- Solutions in clinical medicine must be integrated with improved surveillance of AMR in agriculture, animal health and the environment.
- AMR must no longer be the remit solely of the health sector, but needs engagement from a wide range of stakeholders, representing agriculture, trade and the environment with solutions that balance their often-competing interests.
- International alignment and coordination are paramount in both policymaking and its implementation.
Consider the question “Anti-microbial resistance (AMR) represents an existential threat to modern medicine. What are the factors contributing to AMR? Suggest the measures to deal with it.”
Conclusion
With viral diseases such as COVID-19, outbreaks and pandemics may be harder to predict; however, given what we know about the “silent pandemic” that is AMR, there is no excuse for delaying action.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Antibiotics Resistance
Looming heath crisis in the form of antimicrobial resistance
From UPSC perspective, the following things are important :
Prelims level: Factors responsible for AMR
Mains level: Paper 3- Link between pollution and AMR
Rapidly rising antimicrobial resistance (AMR) poses the threat of the next health crisis if not addressed with urgency. The article examines the severity of the issue.
The severity of the antimicrobial resistance (AMR)
- Globally, about 35% of common human infections have become resistant to available medicines.
- About 700,000 people die every year because available antimicrobial drugs — antibiotics, antivirals, antiparasitic and antifungals — have become less effective at combating pathogens.
- Resistance to second- and third-line antibiotics — the last lines of defence against some common diseases — are projected to almost double between 2005 and 2030.
- In India, the largest consumer of antibiotics in the world, this is a serious problem.
Responsible factors
- Microorganisms develop resistance to antimicrobial agents as a natural defence mechanism.
- Human activity has significantly accelerated the process.
- The misuse and overuse of antimicrobials for humans.
- Livestock and agriculture but other factors also contribute.
Research points to role of environment and pollution
- Once consumed, up to 80% of antibiotic drugs are excreted un-metabolised, along with resistant bacteria.
- Their release in effluents from households and health and pharmaceutical facilities, and agricultural run-off, is propagating resistant microorganisms.
- Wastewater treatment facilities are unable to remove all antibiotics and resistant bacteria.
- In India, there is capacity to treat only about 37% of the sewage generated annually.
- Water, then, may be a major mode for the spread of AMR, especially in places with inadequate water supply, sanitation and hygiene.
- Wildlife that comes into contact with discharge containing antimicrobials can also become colonised with drug-resistant organisms.
Initiative to tackle the AMR
- The United Nations Environment Programme (UNEP) identified antimicrobial resistance as one of six emerging issues of environmental concern in its 2017 Frontiers Report.
- UN agencies are working together to develop the One Health AMR Global Action Plan (GAP) that addresses the issue in human, animal, and plant health and food and environment sectors.
- The Ministry of Environment, Forest and Climate Change (MoEF&CC) issued draft standards which set limits for residues of 121 antibiotics in treated effluents from drug production units.
- The Ministry of Health and Family Welfare and MoEF&CC constituted the inter-ministerial Steering Committee on Environment and Health, with representation from WHO and UNEP.
Way forward
- The Centre and State governments in India can strengthen the environmental dimensions of their plans to tackle antimicrobial resistance.
- It is important to promote measures that address known hotspots such as hospitals and manufacturing and waste treatment facilities.
Consider the question “Being the largest consumer of antibiotics in the world, India faces a grave threat from growing anti-microbial resistance. What are the factors responsible for it? Suggest the ways to deal with it.”
Conclusion
We saw how quickly a pandemic can spread if we are not ready. This is an opportunity to get ahead of the next one.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024











