Medical Education Governance in India
[8th March 2025] The Hindu Op-ed: What ails Pre-Clinical PG Courses?
PYQ Relevance:Q) Appropriate local community level healthcare intervention is a prerequisite to achieve ‘Health for All’ in India. Explain. (UPSC CSE 2018) |
Mentor’s Comment: UPSC mains have always focused on the ‘Health for All’ (2018) and primary health structure is a necessary precondition (2021).
No students enrolled in postgraduate (PG) medical pre-clinical courses like anatomy, biochemistry, physiology, forensic medicine, microbiology, and pharmacology at Vydehi Institute of Medical Sciences and Research Centre (VIMS), Bengaluru, until the second round of PG-NEET counselling.
Today’s editorial discusses the issues related to postgraduate medical seats. This content would help in GS Paper 2 and 3 in the mains paper.
_
Let’s learn!
Why in the News?
Many postgraduate medical seats are vacant this year because students are choosing pre-clinical courses.
Why are postgraduate medical students reluctant to choose pre-clinical courses in Karnataka?
- Lack of Job Opportunities: Pre-clinical graduates cannot practice as doctors and are limited to working in laboratories, diagnostic centers, or as faculty. Example: Despite reducing tuition fees and offering job guarantees, private institutions like the Vydehi Institute of Medical Sciences struggle to fill pre-clinical seats due to limited employment avenues.
- Lower Salary Compared to Clinical Courses: Pre-clinical roles offer significantly lower remuneration than clinical practice, making them financially unattractive. Example: A clinical doctor can earn a higher salary working in hospitals or private practice, while pre-clinical graduates face salary stagnation in academic or lab-based roles.
- Limited Career Progression and Mobility: Clinical course graduates have the flexibility to work globally and in various healthcare sectors, while pre-clinical graduates are restricted to teaching or research roles. Example: An MD in General Medicine can practice as a physician anywhere, whereas an MD in Anatomy primarily qualifies for academic positions.
- High Capital Requirement for Self-Employment: Establishing independent diagnostic centers requires significant investment, which deters pre-clinical graduates from entrepreneurial ventures. Example: Diagnostic centers with advanced technology demand substantial startup costs, making it challenging for pre-clinical graduates to become self-employed.
- Persistent Seat Vacancies Reflect Low Demand: Consistent under-enrollment over the years signals a long-term disinterest in these courses. Example: In 2024-25, only 6 out of 104 MD Anatomy seats were filled in Karnataka, despite five rounds of counselling and reduced cut-off percentages.
What is the trend of student enrollment in PG medical courses at the all-India level?
What is the significance of pre-clinical courses?
|
How has the National Medical Commission (NMC) addressed the issue of unfilled PG medical seats in Karnataka?
- Reduction of NEET-PG Cut-off Scores: In an unprecedented move, the NEET-PG 2023 cut-off was reduced to zero, making all candidates who appeared for the exam eligible for PG medical programs. This decision aimed to expand the pool of eligible candidates and fill vacant seats across various specialties.
- Guidelines for Interstate Posting Under District Residency Programme: The NMC issued directives emphasizing strict adherence to the Post-Graduate Medical Education Regulations, 2023.
- These guidelines facilitate the interstate posting of PG medical students under the District Residency Programme, ensuring a more even distribution of medical professionals and addressing regional disparities in seat occupancy.
- Monitoring and Rectifying Seat Allocation Discrepancies: The NMC has been proactive in addressing discrepancies between its records and those of state authorities. For instance, admissions to 23 PG medical seats in Bengaluru were put on hold due to mismatches between NMC and Directorate of Medical Education (DME) lists. Such actions ensure that seat allocations are transparent and accurate.
- Annual Increase of PG Seats: The NMC has facilitated the process for medical institutions to apply for an increase in PG seats for the academic year 2025-26. By inviting applications and setting clear guidelines, the commission aims to enhance the availability of PG medical seats, thereby reducing the likelihood of vacancies.
Way forward:
- Enhance Pre-Clinical Career Prospects: Introduce incentives like research grants, industry collaborations, and fellowship programs to improve career progression and salary prospects for pre-clinical graduates.
- Targeted Seat Distribution and Quality Monitoring: Implement region-specific seat allocation policies and strengthen regulatory oversight to ensure quality education and equitable access across underserved states.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
[6th March 2025] The Hindu Op-ed: Over-centralisation threatens federal health policy
PYQ Relevance:Q)Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (UPSC CSE 2021) |
Mentor’s Comment: UPSC mains have always focused on the Welfare State, primary health structure (2021), and Public health system (2015).
The Supreme Court’s judgment in Dr. Tanvi Behl vs Shrey Goyal (2025), striking down domicile-based reservations in post-graduate medical admissions, changes India’s medical education policy. While promoting merit, it overlooks how these reservations support State public health needs and may discourage States from investing in government medical colleges, weakening their healthcare systems.
Today’s editorial discusses domicile-based reservations, which is useful for writing answers in UPSC Mains GS Paper 2 on Governance, especially regarding State policies and public health challenges.
_
Let’s learn!
Why in the News?
The ruling that ended domicile-based reservations in post-graduate medical admissions ignores the practical challenges of managing public health.
What are Domicile-based reservations?
|
What are the key arguments made by the Supreme Court in striking down domicile-based reservations?
- Violation of Article 14 (Right to Equality): The Court held that domicile-based reservations in post-graduate medical admissions violate Article 14 of the Constitution, which guarantees equality before the law. Example: It argued that restricting access to medical seats based on domicile status is discriminatory against equally qualified non-local candidates.
- Primacy of Meritocracy in Higher Education: The judgment emphasized that merit should be the primary criterion for post-graduate medical admissions to ensure the best candidates receive specialist training. Example: It relied on Pradeep Jain vs Union of India (1984), where the Court discouraged domicile-based quotas, stating that such policies dilute academic standards in advanced medical training.
- Uniform and Centralized Medical Education Framework: The Court favored a national, merit-based system to maintain uniformity in medical admissions across States and prevent fragmentation. Example: It pointed to central institutions like AIIMS and PGIMER, which follow a centralized selection process without domicile reservations, ensuring open competition for all candidates.
Why is domicile-based reservation considered crucial for State-level?
- Retention of Specialist Doctors in Public Health Systems: Domicile quotas ensure that medical graduates trained in State institutions are more likely to serve within the State, addressing local health-care needs. Example: States with severe specialist shortages (e.g., rural Bihar or Odisha) rely on domicile-based reservations to retain medical professionals and improve health outcomes.
- Alignment of State Investment with Local Workforce Needs: States invest substantial resources in medical education and expect returns through a local medical workforce. Domicile quotas ensure these investments benefit the State’s health infrastructure. Example: Tamil Nadu links domicile-based quotas to mandatory public service, ensuring that doctors trained using State funds serve in government hospitals.
- Addressing Regional Health Disparities: Domicile reservations help in reducing regional imbalances by ensuring that underserved areas have access to medical specialists who understand local challenges. Example: Northeastern States with limited access to advanced medical care use domicile quotas to maintain a local pool of doctors familiar with tribal and rural health needs.
- Predictable Medical Workforce Supply: States depend on domicile quotas to create a steady pipeline of medical specialists who can fulfill long-term public health needs. Example: Maharashtra implements domicile-based reservations to ensure consistent recruitment for rural health centers and district hospitals.
- Incentivizing State Investment in Medical Education: If States cannot ensure that their medical graduates remain local, they may reduce funding for medical colleges, weakening health infrastructure. Example: Without domicile quotas, smaller States like Goa risk losing locally trained doctors to other regions, discouraging future investment in medical education.
How does the ruling impact State incentives to invest in government medical colleges and public health infrastructure?
- Reduced Motivation to Fund Medical Education: Without domicile-based reservations, States cannot ensure that doctors trained in government-funded colleges will stay and serve locally. This may discourage future investments in medical education. Example: Odisha may be less inclined to invest in new medical colleges if graduates move to other States for better opportunities.
- Weaker Public Health Infrastructure: States depend on locally trained doctors to staff public hospitals. Without a guaranteed local workforce, rural and underserved areas may face doctor shortages, weakening health services. Example: Bihar, already struggling with a lack of specialists, could face further shortages in district hospitals due to reduced local retention.
- Increased Dependence on External Recruitment: The ruling forces States to rely on recruiting doctors from outside, which can be costly, inefficient, and unpredictable, especially in remote regions. Example: Himachal Pradesh may need to import specialists, increasing costs and reducing long-term staffing stability in rural clinics.
- Discouragement of Regional Policy Innovation: States using service-linked quotas to address local health needs lose a valuable tool to customize their medical education policies. Example: Tamil Nadu’s model, which ties post-graduate seats to public service, could be undermined, reducing the State’s ability to ensure healthcare delivery.
- Widening Regional Health Inequalities: States with fewer resources will struggle to compete with wealthier regions in attracting and retaining medical professionals, increasing healthcare gaps. Example: Northeastern States like Assam may face a brain drain, making it harder to deliver essential medical care in rural areas.
Way forward:
- Balanced Policy Framework: Introduce a hybrid model combining merit-based admissions with incentives (e.g., service bonds or rural postings) to retain doctors in underserved areas while upholding constitutional equality.
- Strengthening National and State Collaboration: Foster State-Centre cooperation to create region-specific policies under the National Medical Commission (NMC) that address local health needs without violating merit-based norms.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
[14th February 2025] The Hindu Op-ed: The problematic globalisation of medical education
PYQ Relevance:Q) Public health system has limitation in providing universal health coverage. Do you think that private sector can help in bridging the gap? What other viable alternatives do you suggest? (UPSC CSE 2015) |
Mentor’s Comment: UPSC mains have always focused on the Public health system (2015), and the Health for All’ in India (2018).
Medical education is changing in unusual ways. There is a shortage of doctors, yet governments and medical professionals limit access to medical studies. As a result, more students from different countries travel abroad to study medicine. In the past, medical education was international, but now each country controls it while it still becomes more global. This trend is important because of healthcare needs. The exact number of students studying medicine abroad is unknown, but it is estimated to be over 200,000, often in low-quality institutions. Before the Russian invasion, Ukraine had 24,000 foreign medical students, mostly from India.
Today’s editorial talks about issues in the Medical sector. This content would help in GS Papers 1, 2 and 3 to substantiate your answer.
_
Let’s learn!
Why in the News?
Studying medicine abroad is common, but it is largely unnoticed and lacks proper regulation.
How does the globalization of medical education impact the quality and accessibility of healthcare?
- Increased Access to Medical Education but Quality Concerns Persist: India has only 1 medical seat for every 22 applicants, with 2.3 million students appearing for NEET annually.
- As a result, over 20,000 Indian students go abroad for medical studies each year. While foreign education provides an alternative, some countries have lax regulatory frameworks, leading to concerns over clinical training standards.
- Low Licensing Exam Pass Rates for Foreign Medical Graduates: India’s Foreign Medical Graduate Examination (FMGE) pass rate has historically been below 20%.
- In 2022, only 10,500 out of 41,349 candidates (25.4%) cleared the exam. Many foreign-trained doctors struggle to meet national standards, delaying their entry into the healthcare system.
- Disproportionate Dependence on Foreign-trained Doctors in Some Countries: In the US, 25% of physicians are international medical graduates (IMGs), while in the UK, 37% of doctors in the NHS come from abroad.
- While globalization helps address doctor shortages in developed countries, it exacerbates the “brain drain” in source countries like India, Nigeria, and Pakistan.
- Growth of For-profit Medical Schools with Limited Oversight: The Caribbean region alone has over 50 private medical schools, many catering exclusively to international students from the US and Canada.
- These institutions charge high tuition fees but often lack sufficient clinical training infrastructure, raising concerns about graduate competence.
- Shortage of Trained Doctors in Source Countries: The WHO estimates a global shortfall of 10 million healthcare workers by 2030, with Africa facing a deficit of 6 million doctors and nurses.
- Many doctors trained abroad do not return home, worsening healthcare shortages in low-income countries while benefiting high-income nations.
What are the consequences of medical degrees that are obtained abroad, especially from countries with lower academic standards?
- High Failure Rates in Licensing Exams: Foreign-trained doctors often struggle to meet national medical standards, leading to low pass rates in licensing exams.
- Example: In India, the Foreign Medical Graduate Examination (FMGE) pass rate has historically been below 20%. In 2022, only 10,500 out of 41,349 candidates (25.4%) cleared the exam, delaying their entry into the healthcare system.
- Limited Clinical Exposure and Skill Gaps: Some foreign medical colleges lack proper clinical training, affecting students’ hands-on experience in diagnosing and treating patients.
- Example: Several Caribbean medical schools, catering to US and Canadian students, have faced criticism for their limited hospital affiliations, forcing students to complete clinical rotations in different countries.
- Difficulty in Securing Residency and Employment: Graduates from lesser-known foreign institutions often struggle to secure postgraduate training and jobs in competitive healthcare markets.
- Example: In the United States, international medical graduates (IMGs) face higher rejection rates for medical residencies, with only about 60% of non-US IMGs matching into residency programs in 2023, compared to 93% of US medical graduates.
Is the global mobility of medical education sustainable, and how does it affect local health systems?
- Brain Drain Weakens Healthcare in Source Countries: Many doctors trained abroad do not return, leading to a shortage of medical professionals in their home countries.
- Example: Nigeria loses over 2,000 doctors annually to migration, worsening its doctor-to-patient ratio, which stands at 1:5,000, far below the WHO-recommended 1:1,000.
- Unequal Distribution of Healthcare Professionals: High-income countries attract foreign-trained doctors, leaving rural and underserved regions in low- and middle-income nations critically short-staffed.
- Example: In India, only 20% of doctors serve in rural areas, even though 65% of the population resides there, leading to severe healthcare disparities.
- Reliance on Foreign-trained Doctors in Host Countries: Developed nations depend on foreign medical graduates to fill workforce gaps, making their healthcare systems vulnerable to changing immigration policies.
- Example: The UK’s NHS workforce includes 37% foreign-trained doctors, with a significant number from India and Pakistan.
Way forward:
- Strengthening Domestic Medical Education Infrastructure: Increase the number of medical seats and improve the quality of training in home countries to reduce dependence on foreign institutions. Example: India has added over 100 new medical colleges since 2019 to expand access to medical education.
- Stricter Accreditation and Recognition of Foreign Medical Degrees: Establish global accreditation standards and bilateral agreements to ensure only high-quality foreign medical degrees are recognized. Example: The National Exit Test (NExT) in India will standardize assessment for both domestic and foreign medical graduates.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
NTA Reform Panel to Check Irregularities in Exams
From UPSC perspective, the following things are important :
Prelims level: NTA
Why in the News?
A seven-member high-level committee was constituted under the chairmanship of K. Radhakrishnan, former ISRO Chairman, by the Ministry of Education to reform the National Testing Agency (NTA).
About National Testing Agency (NTA)
|
National Testing Agency (NTA) Under Scrutiny
- The NTA has been criticized after the NEET paper leak controversy and the subsequent scrapping of exams like UGC-NET due to “lack of integrity”.
- The committee aims to establish a robust process for conducting various entrance examinations end to end.
NTA Reform Panel: Committee Composition
- Committee Head: K. Radhakrishnan, former Chairman of ISRO and Chairman of the Board of Governors at IIT-Kanpur.
- Two-Month Timeline: The committee aims to meet ten times over the next two months to develop comprehensive recommendations.
- Key Issues and Focus Areas:
- Data Security Protocol: Develop a manual to fix a data security protocol to prevent question paper leaks.
- Printing and Process Integrity: Review processes for printing question papers, onboarding printers, and training staff to minimize external participation.
- Organisational Restructuring: Consider adding a data security vertical in the NTA organogram and implementing transparent processes, requiring organizational restructuring.
- Examination Investigation and Security:
- Root Cause Analysis: The committee will investigate the initial cause of question paper leaks to identify and plug gaps.
- Modes of Examination: Examine different modes of conducting examinations:
- JEE (Mains) and JEE (Advanced) are computer-based tests.
- NEET-UG is conducted in pen-paper Optical Mark Recognition (OMR) mode.
Challenges faced by NTA
- Infrastructure Limitations: Currently, India lacks the infrastructure to conduct computer-based tests online for more than three lakh students simultaneously.
- Large-Scale Exams: NEET-UG involves up to 24 lakh students appearing in pen and paper OMR mode at once.
Conclusion
- The reforms are critical to restoring the integrity of entrance examinations in India, ensuring secure and fair testing processes.
- The committee’s recommendations will play a pivotal role in shaping the future operations of the NTA and entrance examination protocols.
Back2Basic: University Grants Commission (UGC)
|
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
The allegations over NEET-UG 2024 | Explained
From UPSC perspective, the following things are important :
Prelims level: NEET, NTA
Mains level: The National Testing Agency responds to the various charges against the conduct of the exams.
Why in the news?
On June 13, the Union government informed the Supreme Court that the scorecards of 1,563 candidates who received compensatory marks in the NEET-UG 2024 exam, held on May 5, will be cancelled.
About National Testing Agency:
|
Why has the Union government told the Supreme Court that it will cancel the scorecards of candidates who have been awarded grace marks?
- Technical Issues During Exam: The cancellation stems from petitions challenging the award of grace marks to 1,563 candidates from six NEET centers due to technical issues that did not allow them the full 3.2 hours to complete the exam.
- Compensatory Marks Controversy: Grace marks were awarded based on a court order and the recommendation of a committee constituted by the National Testing Agency (NTA). This move was challenged as arbitrary and lacking transparency.
- Skewed Results: The committee found that the compensatory marks led to a skewed situation, thus recommending the cancellation of the scorecards for these candidates and conducting a re-test on June 23.
How did the National Testing Agency respond to the various charges against the conduct of the exams?
- Formation of Committee: In response to the allegations, the NTA constituted a four-member committee to investigate the truth behind the claims, including the award of grace marks and other issues related to the conduct of NEET 2024.
- Admission of Irregularities: The NTA admitted that the grace marks caused confusion and contributed to skewed results. They acknowledged technical issues and the improper awarding of grace marks.
- Panel Recommendations: The panel recommended limiting grace marks to the attempted questions and concluded that it would be best to cancel the test for the affected 1,563 students.
- Explanations for High Scores: NTA officials attributed the unusually high number of perfect scores (67 students scoring 720/720) to an ‘easy paper’, but still took steps to address the fairness and validity of the results by planning a re-test.
- Addressing Other Allegations: The NTA’s response included acknowledging various logistical issues such as slow distribution of question papers, wrong OMR sheets, and technical delays, and they aimed to ensure better planning and execution in future exams.
Way forward:
- Calls for a Re-test for All Candidates: Students and education experts argue that if the exam can be cancelled for 1,563 candidates, it should be cancelled for all 23 lakh candidates to maintain fairness. They believe that the logical step is to conduct a re-test for everyone who took the May 5 exam.
- Restoring Faith in the System: The dissatisfaction expressed on social media highlights a loss of faith in the examination system. To restore confidence, students demand comprehensive measures to address the flaws and ensure a fair and transparent testing process for all candidates.
- Improving Examination Conduct: For an exam of NEET’s scale and history, it is expected that organizational issues should be resolved. The NTA and government agencies need to enhance measures to prevent fraud, ensure the timely distribution of materials, and apply proper judgment to address any technical issues during the exam, aiming for a smooth and reliable process in future examinations.
Mains PYQ:
Q National Education Policy 2020 is in conformity with the Sustainable Development Goal-4 (2030). It intends to restructure and reorient the education system in India. Critically examine the statement. (UPSC IAS/2020)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
SC to reconsider its 1995 judgement to include the medical profession under the Consumer Protection Act
From UPSC perspective, the following things are important :
Prelims level: Judiciary; Consumer Protection Act (CPA)
Mains level: Judiciary; Judicial overreach; Consumer Protection Act (CPA)
Why in the news?
Recently, the apex court held that lawyers as ‘professionals’ could not be subjected to legal proceedings for providing faulty ‘service’ under the Consumer Protection Act 2019 (CPA). A similar case applies to Medical practitioners which is in high controversy.
What is the Consumer Protection Act (CPA)?
| Consumer Protection Act, 1986 | Consumer Protection Act, 2019 | |
|---|---|---|
| Purpose | Enacted to provide simpler and quicker access to redressal of consumer grievances. | Repeals and replaces the CPA, 1986. |
| Introduction of Concept | Introduced the concept of ‘consumer’ and conferred additional rights on consumers. | Expands the scope of the definition of ‘consumer’ to include transactions conducted offline or online through electronic means, teleshopping, direct selling, or multi-level marketing. |
| Scope of Protection | Protects individuals fitting the definition of ‘consumer’ as defined by the Act. | Extends protection to a wider range of transactions, including those related to banking, insurance, transport, housing construction, entertainment, amusement, etc. |
About the previous case – Indian Medical Association vs V P Shantha (1995):
- In 1995, a three-judge bench of the SC ruled, “Doctors would be covered under the consumer protection law, allowing the filing of several medical negligence lawsuits against doctors for deficiency in service”.
- The court also acknowledged that medical professional occupations are often “skilled” work which differs from other occupations and the success usually depends on factors that are beyond the doctor’s control.
Diversity of present Opinions:
- What did the National Consumer Disputes Redressal (NCDR) Commission say?
-
-
- In 2007, the NCDR Commission held that lawyers provide a service to their clients and hence they can be sued for deficiency of service.
- This case ultimately reached the apex court where the judgement was passed recently.
-
- What did the Apex court say?
-
- The court said that the objective principle of the CPA 2019 was to protect consumers from unfair trade practices and unethical business practices (the law was not intended to include professionals).
- The court noted that the legal profession is unique and cannot be compared with any other profession.
- According to the SC, hiring or availing of an advocate is “a contract of personal service” and is therefore exempted from the scope of the consumer protection law.
About the Consumer Redressal Commissions in India:
|
Why does the Apex Court not Exempt Medical Profession from the Purview of CPA?
- Firstly, doctors have specific duties to their patients, such as deciding on treatment and its administration.
- Secondly, if a doctor breaches these duties by failing to provide a reasonable standard of care, they can be held liable under the CPA.
- Additionally, the court believes requiring commission members to have case-specific knowledge would be impractical and burdensome.
Conclusion: This decision aims to prevent potential imbalances between District and State Commissions in handling cases and places the responsibility on parties to provide evidence for informed decisions.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Issues facing Medical Colleges in India
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: Medical colleges, significance, myths, challenges and and comprehensive healthcare
What’s the news?
- In Kerala, a case of medical negligence involving a forgotten surgical instrument inside a patient and increasing vacancies in dental courses across the nation’s colleges spotlight the efficacy and responsibilities of medical institutions in India’s healthcare system.
Central idea
- The rising incidents of medical negligence in leading Indian medical colleges and the Union Government’s 2019 Policy Proposal, which aims to convert district hospitals into medical colleges and establish AIIMS-like institutions in every state, prompt a revaluation of medical colleges’ contribution to patient care from a public health perspective.
The government’s proposal
- Conversion of District Hospitals: The government aims to convert district hospitals across the country into medical colleges. District hospitals are typically considered to be at a secondary level of healthcare, and this policy suggests upgrading them to medical colleges, which are institutions for medical education and training.
- Establishment of AIIMS-like Institutions: The government also intends to establish institutions similar to the AIIMS in every state. AIIMS is renowned for providing advanced healthcare services, medical education, and research. The objective is to replicate AIIMS-like facilities in each state to enhance medical infrastructure and education.
Purpose of a medical college
- Educational Role:
- The foremost purpose of a medical college is to provide education and training to students aspiring to become medical professionals.
- This involves imparting the theoretical knowledge, practical skills, and clinical experiences necessary for students to become competent healthcare practitioners.
- Medical Care:
- A secondary purpose of a medical college is to offer medical care. This is facilitated through the associated medical college hospital, which is equipped with state-of-the-art facilities.
- The hospital serves as a platform for the practical training and apprenticeship (internship) of medical students.
- It provides bedside care, an essential requirement for medical training, and contributes to the development of clinical skills.
Myths related to medical colleges
- Myth of Comprehensive Healthcare: There’s a misconception that having a medical college in a district can address all healthcare needs, which can lead to an overestimation of the capabilities of medical colleges.
- Myth of Increased Medical Seats: Establishing a medical college is often associated with the belief that it will increase the availability of medical seats for local students, creating a false hope for aspiring medical professionals.
- Myth of Quantity Over Quality: There’s a misconception that producing more medical professionals will automatically resolve issues related to inadequate healthcare access, overlooking the importance of quality healthcare provision.
- The Myth of Tertiary Care Solving All Issues: The belief that tertiary care services offered by medical colleges can cater to all healthcare needs may undermine the significance of strengthening primary and secondary care services.
- The Myth of Medical Colleges as Ideal Solutions: The notion that medical colleges are the ultimate solution to healthcare challenges might oversimplify the complexities of healthcare delivery, particularly in areas where secondary-level care can have a significant impact.
|
Back to basics
|
Challenges faced by medical colleges in healthcare delivery
- Patient Overload: Higher-level medical facilities, including medical colleges, experience a heavy influx of patients seeking primary and secondary care, leading to patient overcrowding.
- Mismanagement of Cases: A significant majority (over 80%) of cases treated in medical colleges are inappropriate for specialized tertiary care, suggesting a mismatch between patient needs and provided services.
- Deficient Referral System: The absence of an effective referral system in India’s healthcare setup results in patients needing primary and secondary care seeking treatment at medical colleges, causing strain.
- Resource Constraints: The varied patient influx, spanning primary to advanced cases, overburdens the resources and infrastructure of medical colleges, potentially affecting care quality.
Examining tertiary care needs and challenges in district healthcare
- It’s a well-established fact that approximately 1% of the total population annually requires advanced tertiary care.
- For instance, in a district with a population of three million, this translates to a demand for 575-700 specialized beds (considering 100%-85% bed occupancy).Most district hospitals are intended to address this specialized tertiary care need.
- However, the challenge arises as district hospitals, expected to operate and follow referral systems from lower-level facilities, face obstacles due to deficient infrastructure, a shortage of specialists, and a lack of referral systems. These issues are exacerbated by the non-functionality of secondary-level care facilities.
Way forward
- Redefine Priorities: Rather than assuming that medical colleges alone can address the diverse healthcare needs of a population, a shift in perspective is required. The primary focus should be on strengthening secondary-care facilities, particularly district hospitals, which can cater to a wider spectrum of curative care requirements.
- Enhance Referral Systems: Implementing and reinforcing efficient referral systems from primary healthcare centers to well-equipped district hospitals can help streamline patient care.
- Balance Educational and Practical Needs: While medical education remains crucial, a stronger emphasis on hands-on training within well-functioning hospitals is essential.
- Strategic Resource Allocation: When contemplating new medical college establishments, a strategic approach is vital. Focus resources on areas with existing infrastructure, connectivity, and clinical facilities to ensure the institution’s viability and effectiveness.
- Community Education and Awareness: To manage expectations and dispel myths, community engagement is paramount. Educate the public about the specific roles and capabilities of medical colleges, preventing false perceptions of comprehensive healthcare solutions.
- Tailored Regional Approaches: Recognize that diverse regions have distinct challenges. Tailor the establishment and operation of medical colleges to local needs, acknowledging that a standardized approach may not effectively address unique community requirements.
- Elevate District Hospitals: District hospitals should receive substantial support, including infrastructure upgrades, specialist staffing, advanced equipment, and improved connectivity. These efforts will bolster secondary-care facilities, reducing the load on higher-level medical institutions.
Conclusion
- The solution lies in dismantling myths and embracing pragmatic strategies. A reimagined healthcare system built upon patient-focused principles will not only fulfill the curative care needs of the populace but also redefine the role of medical colleges as beacons of comprehensive healthcare.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Tamil Nadu vs. NEET: Balancing Equity and Autonomy
From UPSC perspective, the following things are important :
Prelims level: Seventh Schedule, NEET
Mains level: Read the attached story
Central Idea
- The conflict between Tamil Nadu and the Centre over the National Eligibility and Entrance Test (NEET) has intensified.
- It has reignited discussions about the transfer of education back to the State List of the Seventh Schedule of the Constitution.
Why in news?
- Educational Autonomy: Chief Minister M.K. Stalin called for education’s transfer back to the State List, originally placed in the Concurrent List during the Emergency.
- NEET Controversy: Tamil Nadu’s opposition to NEET escalated dramatically after the tragic suicides of a student and his father due to exam-related stress.
Why Tamil Nadu Opposes NEET?
- Undue competition: NEET, a centralised entrance exam for medical courses, faces opposition in Tamil Nadu due to its mechanical focus on marks.
- Impact on Local Models: NEET disrupted models like Christian Medical College (CMC) Vellore, known for emphasizing aptitude over marks.
- In-Service Quota Impact: NEET dismantled Tamil Nadu’s in-service quota for medical graduates, adversely affecting healthcare quality.
- Disadvantages Marginalized: The exam favours affluent sections who affords lakhs worth coaching (esp. repeaters), disadvantaging underprivileged groups and hindering their aspirations.
Emotive Nature of the Issue
- Equity and Social Justice: Opposition to NEET is deeply rooted in demands for educational equity and autonomy, driven by social justice concerns.
- Kamaraj’s Vision: Tamil Nadu’s education vision, shaped by Chief Minister K. Kamaraj, emphasized accessibility and empathy for unlettered masses.
Legislative Struggles
- AIADMK Bills: The previous AIADMK government introduced Bills in 2017 seeking state autonomy in medical admissions. They were returned by the President.
- Stalin’s Efforts: In 2021, CM M.K. Stalin’s government passed the Tamil Nadu Admission to Undergraduate Medical Degree Courses Bill, 2021, aiming to abolish NEET and base admissions on Class 12 marks for social justice.
- Governor’s Opposition: Governor R.N. Ravi, opposed to the anti-NEET Bill, delayed its forwarding to the President, leading to political tensions.
Justice A.K. Rajan Committee
- Committee Formation: The Justice A.K. Rajan Committee was established in 2021 to assess NEET’s fairness in medical admissions.
- Critical Findings- Rich vs. Poor: The committee criticized NEET for favouring repeaters and coached students while disadvantaging first-time applicants, leading to reduced admissions among marginalized groups.
Why is TN now fuming?
- Concurrent List: Medical course admissions fall under the Concurrent List (Entry 25), allowing states to legislate on these matters.
- Amending Central Laws: States can enact laws related to admissions and amend central laws on admission procedures, as long as they don’t contradict parliamentary laws.
Current Scenario
- Historic Public Health Practices: Tamil Nadu’s public health infrastructure thrived on retaining PG doctors, indicating the state’s effective healthcare practices.
- Balancing Uniformity and Fairness: The NEET stalemate reflects the challenge of balancing uniformity with local values and needs.
- Clash of Values: The conflict highlights the broader tension between central standardization and local autonomy, revealing deeper debates about democracy, equality, and social justice in India.
Conclusion
- The NEET controversy in Tamil Nadu is not merely about an entrance exam; it represents a larger struggle for educational equity, autonomy, and social justice.
- The state’s commitment to its unique vision of education and healthcare clashes with central standardization, sparking a crucial dialogue about the nature of democracy and fairness in the country.
Back2Basics: Seventh Schedule
- The Seventh Schedule under Article 246 of the Indian Constitution is a pivotal component that delineates the allocation of powers between the central government and the states.
- This framework ensures an efficient governance structure by classifying subjects into three lists:
- Union List: The Union List outlines subjects on which only the Parliament can legislate. This list includes crucial aspects like defense, foreign affairs, currency, communication, and more.
- State List: The State List enumerates matters solely under the jurisdiction of state legislatures. It encompasses areas such as public health, agriculture, police, local government, and others.
- Concurrent List: The Concurrent List incorporates subjects on which both Parliament and state legislatures can enact laws. However, in case of a conflict, federal supremacy grants authority to the Parliament’s law.
Evolution and Dynamics
- Over time, the Union List expanded to encompass significant areas such as defense, banking, and foreign affairs.
- The State List’s scope included subjects like public order, police, and agriculture, critical for regional governance.
- The Concurrent List reflects matters of shared importance like criminal law, civil procedure, population control, and more.
Amendments and Special Provisions:
- 42nd Amendment Act (1976): It transferred select subjects like education, forests, and administration of justice from the State List to the Concurrent List.
- 101st Amendment Act (2018): It introduced a special provision for Goods and Services Tax (GST), allowing both Parliament and state legislatures to make laws regarding GST.
Power Distribution and Conflict Resolution:
- Parliament’s jurisdiction prevails over the State List and the Concurrent List in cases of overlap.
- In cases of overlap between the Union List and the State List, the Union List takes precedence.
- If there’s a conflict between the Union List and the Concurrent List, the Union List prevails.
- In situations of conflict between central and state laws on a Concurrent List subject, central law prevails. An exception exists if the state law has the president’s assent.
Consultative Approaches
- Sarkaria Commission (1983) recommended maintaining the existing list allocation, emphasizing the absence of a strong case for transferring items from the Concurrent List to the State List.
- Venkatachaliah Commission (2002) underscored the lack of a formal institution requiring consultation between the Union and states while legislating under the Concurrent List.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Examining the Viability of The Proposal Three-Year Diploma Course for Rural Medical Practitioners
From UPSC perspective, the following things are important :
Prelims level: Medical education related reforms in news
Mains level: A three-year diploma course for rural medical practitioners, arguments in favour and criticism and a way forward
Central Idea
- West Bengal Chief Minister Mamata Banerjee’s proposal to introduce a three-year diploma course for medical practitioners, who would then serve in primary health centers (PHCs), has sparked a debate on its potential impact. While some argue that it could address the shortage of doctors in rural areas, others express concerns about the adequacy of training and the potential erosion of the medical education structure.
What is the proposal is all about?
- The proposal put forth by West Bengal Chief Minister Mamata Banerjee suggests the introduction of a three-year diploma course for medical practitioners.
- The aim of this proposal is to address the shortage of doctors in rural areas by training individuals who would then serve in primary health centers (PHCs) in those regions.
- The idea is to provide basic healthcare services to rural populations by creating a cadre of medical practitioners who are specifically trained for this purpose.
What are the reasons behind such proposal?
- Shortage of Doctors in Rural Areas: Despite having a significant number of MBBS seats in India, there continues to be a severe shortage of doctors in rural areas. Many doctors prefer to practice in urban areas, leaving rural populations underserved.
- Aversion to Rural Practice: There exists a general aversion among doctors to practice in rural areas due to various reasons, such as limited infrastructure, lack of amenities, and professional isolation. This aversion contributes to the scarcity of healthcare providers in rural regions.
- Access to Basic Healthcare: Rural populations often face challenges in accessing basic healthcare services due to geographical barriers, lack of transportation, and inadequate healthcare infrastructure. Introducing trained medical practitioners in rural areas can improve the availability and accessibility of healthcare services for these communities.
- Cost and Recruitment Challenges: Recruiting and retaining fully qualified doctors in rural areas can be costly and challenging. The proposal for a three-year diploma course aims to provide a more feasible and practical solution by training healthcare professionals who can handle primary healthcare needs and work in rural settings.
- Inequity in Healthcare: There is a concern about the inequitable distribution of healthcare resources, with urban areas receiving more qualified doctors compared to rural areas. It attempts to address this inequity by deploying medical practitioners specifically trained for rural healthcare, ensuring that rural populations receive adequate medical attention.
Arguments in favour of the proposal
- Addressing Doctor Shortage: The primary benefit of the proposal is that it can help alleviate the acute shortage of doctors in rural areas. By training medical practitioners specifically for rural healthcare settings, the proposal aims to ensure that these underserved regions have access to basic healthcare services.
- Cost-Effective Solution: Compared to recruiting fully qualified doctors to rural areas, implementing a three-year diploma course can be a more cost-effective solution. It allows for the training of healthcare professionals who possess the necessary skills to handle primary healthcare needs in rural settings without the extensive training period required for a full-fledged medical degree.
- Improving Healthcare Accessibility: Introducing trained medical practitioners in rural areas improves the accessibility of healthcare services for the rural population. By having healthcare providers available locally, rural communities can receive timely medical attention without the need to travel long distances to urban areas, particularly for primary healthcare needs.
- Filling Immediate Healthcare Needs: The proposal aims to bridge the immediate gap in healthcare by deploying medical practitioners who can handle non-critical situations effectively. These practitioners can provide essential medical care, diagnose common ailments, offer preventive services, and refer critical cases to higher-level healthcare facilities.
- Reducing Disparity: The proposal seeks to reduce the disparity between rural and urban healthcare by ensuring that rural populations have access to healthcare professionals who are specifically trained to cater to their needs.
- Incentivizing Rural Practice: By creating a specific cadre of medical practitioners trained for rural areas, the proposal can potentially incentivize doctors to serve in rural settings. It acknowledges the challenges and aversion towards rural practice and offers a tailored training program to prepare healthcare professionals for the realities and demands of working in rural healthcare settings.
- Enhancing Continuity of Care: Deploying trained medical practitioners in rural areas can contribute to the continuity of care. By having a consistent presence of healthcare professionals in rural communities, it ensures that patients receive ongoing medical attention, follow-ups, and necessary treatments, thereby improving healthcare outcomes.
Concerns raised against the proposal
- Inadequate Training and Skills: Critics argue that a three-year diploma course may not provide sufficient training and expertise to deal with the complex healthcare challenges in rural areas. They express concerns that these practitioners may lack the necessary knowledge, experience, and skills to handle emergency situations or provide specialized care required in rural healthcare settings.
- Compromising Quality of Care: There is a concern that employing less qualified practitioners in rural areas may compromise the quality of healthcare provided to rural populations. It is argued that rural communities deserve the same level of medical expertise and care as urban areas. Introducing practitioners with a shorter training period may create disparities in the quality of healthcare between rural and urban regions.
- Professional Discrimination: Critics contend that deploying less qualified practitioners in rural areas can be seen as discriminatory. It implies that rural populations are being provided with lower-quality healthcare professionals compared to their urban counterparts. This approach may perpetuate healthcare inequalities and undermine the principle of equal access to healthcare for all citizens.
- Retention and Continuity of Care: Skepticism arises regarding the retention of healthcare professionals trained through the diploma course in rural areas. Concerns are raised that these practitioners may consider rural service as a stepping stone to more desirable urban positions, leading to a lack of continuity of care in rural communities.
- Impact on Medical Education Structure: Some argue that introducing a separate diploma course for rural practitioners may erode the existing structure of medical education. It may create a parallel system that devalues the full-fledged medical degrees and dilutes the standards of medical education, leading to potential academic discrimination and confusion in the healthcare sector.
- Need for Holistic Solutions: Critics suggest that focusing solely on training mid-level practitioners may not address the underlying issues causing doctor shortages in rural areas. They argue that a comprehensive approach is needed, including incentivizing doctors for rural practice, improving infrastructure, providing support systems, and addressing the social and economic factors that contribute to the aversion toward rural practice.
- Distribution of Medical Colleges: Critics also emphasize the need to address the concentration of medical colleges in certain regions, exacerbating the shortage of doctors in rural areas. Redistributing medical colleges and increasing their numbers in underserved regions could potentially contribute to a more equitable distribution of healthcare resources.
Way forward
- Strengthening Medical Education: Focus on improving the quality of medical education and training to produce doctors who are well-equipped to serve in rural areas. This includes emphasizing rural health components in the curriculum, promoting community-based learning experiences, and fostering a sense of social responsibility among medical students.
- Incentivizing Rural Practice: Implement targeted incentives and benefits to attract doctors to rural areas. This can include financial incentives, career advancement opportunities, preferential admission to post-graduate courses, loan forgiveness programs, and improved working conditions. Such measures can help address the aversion to rural practice and encourage doctors to serve in underserved regions.
- Compulsory Rural Postings: Explore the implementation of mandatory rural postings for medical graduates as a way to ensure a continuous supply of doctors in rural areas. However, adequate support systems should be in place to ensure the well-being and professional growth of doctors during their rural service.
- Strengthening Healthcare Infrastructure: Invest in improving healthcare infrastructure in rural areas, including the establishment and upgrading of primary health centers, sub-centers, and other healthcare facilities. This includes ensuring availability of necessary equipment, medicines, and adequate support staff to enhance the functioning of healthcare services.
- Telemedicine and Technology Integration: Leverage telemedicine and technology solutions to bridge the gap in healthcare access. Telemedicine platforms can facilitate remote consultations, diagnosis, and follow-up care, connecting rural patients with specialists in urban areas. Additionally, technology can aid in data management, resource allocation, and monitoring of healthcare services in rural regions.
- Redistribution of Medical Colleges: Address the concentration of medical colleges in certain regions by redistributing and increasing their numbers in underserved areas. This can help ensure a more equitable distribution of healthcare resources and encourage medical students to practice in rural settings.
- Collaborations and Partnerships: Foster collaborations between government agencies, medical institutions, non-profit organizations, and private sectors to collectively address the challenges of rural healthcare. Collaborative efforts can enhance resource sharing, knowledge exchange, and the implementation of effective strategies to improve healthcare delivery in rural areas
- Community Engagement and Health Awareness: Involve local communities in healthcare decision-making processes, encourage their active participation, and enhance health awareness through community-based programs. This can help empower communities to take charge of their own health, improve preventive practices, and create a supportive environment for healthcare professionals in rural areas.
Conclusion
- While the proposal for a three-year diploma course for rural medical practitioners sparks a debate, it is crucial to strike a balance between addressing the shortage of doctors in rural areas and maintaining the quality of healthcare. Ultimately, a comprehensive and multi-faceted approach is required to ensure accessible and sustainable healthcare services for all sections of society.
Also read:
| Healthcare: Public Health and The Insurance Funding |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
National Exit Test (NExT) for Medical Grads
From UPSC perspective, the following things are important :
Prelims level: NEXT
Mains level: Not Much

Central Idea: The NExT examination, a common qualifying criterion for final-year undergraduate medical students will be introduced in the year 2024.
National Exit Test (NExT)
- Objective: The examination aims to bring uniformity in evaluation across the country, ensuring minimum common standards of education and training for medical graduates.
- Two-Part Examination: The NExT exam will consist of two parts: NExT 1, which will be a theoretical examination, and NExT 2, which will include practical, clinical, and oral examinations covering seven clinical subjects or disciplines.
- Mock Test: A mock test may be conducted to familiarize students with the procedure and alleviate any anxiety before the official examination is rolled out.
National Medical Commission and Application of NExT
- Role of NMC: The NMC is responsible for implementing the NExT examination and ensuring a common standard for medical education in the country.
- Applicability: The NExT examination will also apply to institutes of national importance, including the All India Institutes of Medical Sciences (AIIMS), to maintain uniformity in medical education.
Significance
- Quality professionals: The NExT examination is seen as a means to ensure quality and produce well-trained Indian medical graduates.
- Expert Perspectives: Experts in the medical field have welcomed the move, emphasizing the importance of uniform examination standards and the opportunity for interns to focus on their clinical training.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Ethical Animal Research: Prospects and Challenges
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: Ethical issues in animal research

A proposed measure in Switzerland would have made that country the first to ban medical and scientific experimentation on animals.
What counts as ‘Ethical’ animal research?
- There is no single standard definition of ethical animal research.
- Ethical animal research refers to the use of animals in scientific studies while ensuring that the animals are treated humanely and their welfare is protected.
- It involves balancing the benefits of the research with the potential harm to the animals and minimizing any harm or suffering that the animals may experience.
Issues involved in animal research
- Inhumane treatment: Animals are often not treated humanely and are mishandled throughout the research process, including during transport, housing, and experimental procedures.
- Animal rights ignored: Animal rights advocates argue that animals have inherent rights and should not be used for human purposes. They argue that animals have the right to life, liberty, and freedom from suffering, and that using animals in research violates these rights.
- Animal distress: We should consider animals’ distress. If something is known to be painful in humans, it is assumed to be painful in animals as well.
The 4 R’s of animal research
The 3 R’s encourage scientists to develop new techniques that allow them to replace animals with appropriate alternatives. The principles are summarized as:
- Reduction
- Refinement
- Replacement
- Rehabilitation
Guidelines for animal research
Federal research agencies follow guiding principles in evaluating the use and care of animals in research.
- Empathy for all: One is that the research must increase knowledge and, either directly or indirectly, have the potential to benefit the health and welfare of humans and other animals.
- Minimal use: Another is that only the minimum number of animals required to obtain valid results should be included.
- Minimise pain and distress: Researchers must use procedures that minimize pain and distress and maximise the animals’ welfare.
- Using IT tools: They are also asked to consider whether they could use non-animal alternatives instead, such as mathematical models or computer simulations.
Significance of such guidelines
Ans. Defined protocol
- They have made sure that scientists create protocols that describe the purpose of their research and why animals are necessary to answer meaningful question.
- The protocol must outline how animals will be housed and cared for, and who will care for and work with the animals, to ensure that they are trained to treat animals humanely.
Why is animal research essential?
- Non-invasive study: Animal research benefits both humans and animals. Numerous medical advances exist because they were initially studied in animals.
- Benefits entire wildlife: Animal research has allowed for the eradication of certain diseases in cattle, for example, leading not only to reduced farm cattle deaths and human famine, but also to improved health for wild cattle.
- Veterinarian care: Health care advances for pets – including cancer treatments, effective vaccines, nutritional prescription diets and flea and tick treatments – are also available thanks to animal research.
Way forward
- Specific guidelines for ethical animal research are typically established by national governments.
- Independent organisations also provide research standards.
- Create Institutional Animal Care and Use Committee.
Attempt UPSC 2024 Smash Scholarship Test | FLAT* 100% OFF on UPSC Foundation & Mentorship programs
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Is Medical Education in Hindi Practicable?
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: Promoting Hindi language and associated issues
Context
- The unveiling of the Hindi editions of the first professional MBBS books by Union Home Minister Amit Shah in Bhopal has stirred anti-Hindi agitations, with the Opposition, especially in the South, contending that the move is nothing more than a poll gimmick.
Why medical education should be in local language (Hindi)?
- Example of Non-English countries: Supporters of the move are quoting examples from China, Japan, Ukraine, Russia, and Norway – countries where official languages are the sole medium of instruction in all the technical and non-technical courses.
- Education in mother tongue is effective: If they can do so, why can’t we, they argue, especially as it is an established fact that imparting education in a student’s mother tongue is effective for learning.
Why English is best medium of English education?
- Teaching in local plus English language: Fifty-two medical colleges, out of the total 170 colleges on mainland China, whose graduates can attempt the USMLE (the entrance exam to practice in the US), teach in both Chinese and English. There has been a steep rise in the number of parents interested in enrolling their children – at just three years old – in ESL (English as a Second Language) courses.
- Less resources in Hindi: It is unwise to compare the status of Hindi to Chinese or German, given India’s diversity. Moreover, Hindi, or any other vernacular language, for that matter, offers far fewer resources to support the job-seeking young populace. Learning English, therefore, comes with a promise of roti, kapda, makaan (food, clothes, shelter.)
- Higher demand for English Medium: A few years ago, when newspapers reported on the closing down of government schools in Tamil Nadu, one of the major reasons cited was parents’ preoccupation with English-medium schools – leading them to deny free cash and food and admit their kids to low-end, mediocre English schools, instead.
- English is a great leveller: When it comes to higher education, English is a great leveller, allowing dialogue to continue with the rest of the world. Medicine, as evidence-based as it is, is constantly evolving with the introduction of novel research. Treating cases sometimes requires consulting multiple books, research papers, and journal articles, for which a sound system of translation needs to be established before we can even begin thinking about phasing out English.
- Issue of Translation: The people involved in the translation process spoke of two things, First, instead of “translation”, the books have been transliterated. The medical terminology remains the same; sentences have only been translated for easier reading. That too, in the most mainstream dialect of Hindi. Second, these books are to be used as “bridge books”, and not as replacements for the English ones, designed to address the initial hiccups students are bound to face.
- No clarity on roadmap: The initial announcement also fails to account for the necessary infrastructure. There has been no clarity on whether or how these translations will be incorporated as reading materials, and how they will evolve or change with time. Whether standard books like Harrison and Robbins would also be translated is anyone’s guess. Translating these tomes only once would not suffice as newer editions every three to five years incorporate significant changes.
- Training of teachers and conferences: Professors and other teaching staff would also need to be trained. Most of all, what about medical conferences, the staple of a medical student? Would they be organised in Hindi moving forward?
- Our medical industry is yet to develop: While basing our argument only on language, we often forget that Chinese healthcare is self-sufficient when it comes to research and protocols, or that Germany has primary resources available in their own language. Our focus right now should be to develop primary resources. Our medical industry is at way too nascent a stage to be speaking of language.
Conclusion
- Offering extra evening classes as done by AIIMS, Delhi could have been a better substitute given that the strength of students who struggle with English makes up about one to two per cent of the entire batch. Besides, no strict distinction exists between Hindi and non-Hindi-speaking states as most institutions have a portion of seats that are filled up by a pan-India entrance exam. Our focus should be on quality of education instead of medium of instruction.
Mains Question
Q. Medical education in English is more viable than local language. Explain. Why Government of India Supports the Medical education in Hindi?
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Centre cites law to deny medical seats to Ukraine-returnees
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: Medical education pursuance in foreign and issues

The Centre has told the Supreme Court that the law does not allow undergraduate medical students, who fled the “war-like situation” in Ukraine, to be accommodated in Indian medical colleges.
Which laws is the govt talking about?
- There are no provisions either under the Indian Medical Council Act, 1956, or the National Medical Commission Act, 2019 to accommodate or transfer medical students.
- Till now, no permission has been given by the National Medical Commission to transfer or accommodate any foreign medical students in any Indian medical institute/university.
Why foreign undergraduates are not permitted?
- Absence of law: The extant regulations in India do not permit migration of students from foreign universities to India.
- No backdoor entry: The public notice cannot be used as a back door entry into Indian colleges offering undergraduate courses.
- Merit issue: The students had left for foreign universities for two reasons, poor marks in the National Eligibility cum Entrance Test (NEET) and affordability of medical education in foreign countries.
- High cost: Besides, these students, if admitted in Indian colleges, would again face the problem of affordability.
Why do Indians go abroad for medical studies?
- According to estimates from Ukraine, reported in the media, around 18,000 Indian students are in Ukraine (before Operation Ganga).
- Most of them are pursuing medicine.
- This war has turned the spotlight on something that has been the trend for about three decades now.
Preferred countries for a medical degree
- For about three decades now, Indian students have been heading out to Russia, China, Ukraine, Kyrgyzstan, Kazakhstan, and Philippines to pursue a medical degree.
Hype of becoming a Doctor
- Prestige: The desire to study medicine still holds a lot of value in the Indian community (the other is becoming an IAS officer).
- Shortages of Doctor: In many rural areas, people still look at doctors as god’s incarnate.
- Rarity of opportunity: The lack of equal opportunities exacerbated by the caste factor in the Indian context, has a great deal of impact on the prestige still associated with being a doctor.
- Social upliftment ladder: For years, certain communities were denied the opportunities, and finally they do have a chance at achieving significant educational status.
Why do Indians prefer going abroad?
- No language barrier: The medium of education for these students is English, a language they are comfortable with.
- Affordability: The amount spent on living and the medical degree are far more affordable than paying for an MBBS seat in private medical colleges in India.
- Aesthetics and foreign culture: People are willing to leave their home to study far away in much colder places and with completely alien cultures and food habits.
- Practice and OPD exposure: It broadens students’ mind and thinking, expose them to a whole range of experiences, and their approach to issues and crises is likely to be far better.
Doesn’t India have enough colleges?
(a) More aspirants than seats
- There are certainly far more MBBS aspirants than there are MBBS seats in India.
- In NEET 2021, as per a National Testing Agency press release, 16.1 lakh students registered for the exam, 15.4 lakh students appeared for the test, and 8.7 lakh students qualified.
- As per data from the National Medical Commission (NMC), in 2021-22, there were 596 medical colleges in the country with a total of 88,120 MBBS seats.
- While the skew is in favour of Government colleges, it is not greatly so, with the number of private medical institutions nearly neck-to-neck with the state-run ones.
(b) Fees structure
- That means over 50% of the total seats are available at affordable fees in Government colleges.
- Add the 50% seats in the private sector that the NMC has mandated must charge only the government college fees.
- In fully private colleges, the full course fees range from several lakhs to crores.
(c) Uneven distribution of colleges
- These colleges are also not distributed evenly across the country, with States such as Maharashtra, Karnataka, Tamil Nadu and Kerala having many more colleges.
What about costs?
- The cost factor on both sides of an MBBS degree is significant.
- The costs of an MBBS degree in a Government college tot up to a few lakhs of rupees for the full course, but in a private medical college, it can go up to ₹1 crore for the five-year course.
- In case it is a management seat, capitation fees can inflate the cost by several lakhs again.
- Whereas, an MBBS course at any foreign medical university in the east and Eastern Europe costs far less (upto ₹30lakh-₹40 lakh).
Way forward
- While PM Modi emphasised that more private medical colleges must be set up in the country to aid more people to take up MBBS, medical education experts have called for pause on the aspect.
- If the aim is to make medicine more accessible to students of the country, the path ahead is not in the private sector, but in the public sector, with the Central and State governments’ involvement.
- Starting private medical colleges by reducing the strict standards set for establishing institutes may not actually be the solution to this problem, if we think this is a concern.
Conclusion
- Creating more medical colleges will be beneficial for the country, if access and availability can be ensured.
- This will not be possible by resorting to private enterprise only.
- The State and Central governments can start more medical colleges, as recommended by NITI Aayog, by utilising district headquarters hospitals, and expanding the infrastructure.
- This way, students from the lower and middle socio-economic rung, who are otherwise not able to access medical seats, will also benefit.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Medical education in India
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: Medical education in India
Context
- The increasing population (1.32 billion ) and the occurrence of diseases, demands Indian medical education and the training approach to be modified and ensure enhancing practical clinical skills, than just sticking with predominantly theoretical or classroom training.
- The demand for medicine to be taught in language beside English has been made repeatedly over the years, and was reiterated by union home minister recently.
Definition
- Medical education consists of training aimed at ensuring physicians acquire the competencies, skills and aptitudes that that allow them to practice professionally and ethically at the highest level.
Goal of medical education
- The goal of basic medical education is to ensure that medical students have acquired the knowledge, skills, and professional behaviors that prepare them for a spectrum of career choices, including, but not limited to, patient care, public health, clinical or basic research, leadership and management, or medical education.
Why medical education in India needs urgent reforms
- Current Status: Despite being home to one of the oldest medicinal systems in the world, India is still struggling to bring its medical education at par with the leaders around the world. The 541 medical colleges in the country haven’t been able to reach the standard of education that could meet the healthcare needs of the country.
- Deficiency: The doctor-patient ratio of 1:1655 in India as against WHO norm of 1:1000 clearly shows the deficit of MBBS. While the government is working towards a solution and targeting to reach the required ratio, there is a need to relook at the overall medical education.
- Post pandemic scenario: The lag in formal medical education has come up evidently post-pandemic when the nation saw the medical fraternity struggling to fill the doctor deficit.
- Structural issues: It also brought forth the outdated learning methods that most of the medical institutes were using. Due to lockdown and fear of Covid-19 spread, a lot of institutes cancelled lectures and practical sessions.
Current challenges faced by medical education in India
- Limited government seats: The number of seats available for medical education in India is far less than the number of aspirants who leave school with the dream of becoming doctors.
- What data speaks: Of the 1.6 million students who appeared in the National Eligibility cum Entrance Test (NEET) in 2021, only 88,120 made it into the 562 medical colleges in the country. Others had to enrol in non-medical courses in India or seek admission to foreign medical colleges. While the number of medical colleges has now increased to 596 (with 89,875 seats), the entry barrier is still high.
- Lack of skills: Though the institutes are managing to hire professors and lecturers, there is a lack of technical skills. Finding faculties in clinical and non-clinical disciplines is difficult and there are very few faculty development programs for upskilling the existing lot.
- Lack of infrastructure: The gap in digital learning infrastructure is currently the biggest challenge the sector is facing. There is an urgent need to adopt technology and have resources available to facilitate e-learning.
- Lack of research and innovation: The medical research and innovation needs an added push as there haven’t been many ground-breaking research here. The education system needs to focus more on increasing the quality of research. Additionally since industry academia partnership is not available, hence innovation also takes a back-seat.
A recent analysis estimates that India has only 4.8 fully qualified and actively serving doctors per 10,000 population.
Government steps in tackling these challenges and issues
- NMC bill: The National Medical Commission Bill, 2019 was passed recently by the parliament. The bill sets up the National Medical Commission (NMC) which will act as an umbrella regulatory body in the medical education system. The NMC will subsume the MCI and will regulate medical education and practice in India. Apart from this, it also provides for reforms in the medical education system.
- MCI suggestion: The Medical Council of India (MCI) launched the globally recognized Competency-based medical education (CBME) for MBBS students in 2019. The CBME curriculum seeks to step away from a content-based syllabus and more towards one that is more practical and aligned with the country’s increasing health demands.
- Schemes: 22 new All India Institutes of Medical Sciences (AIIMS) were developed under this initiative, and MBBS classes have already commenced at 18 of the new AIIMS.
About NMC
|
Steps to be taken
- To cater to any unprecedented demand in the future and to bring up the quality of education, the Indian medical education system undoubtedly needs major reforms.
- While the focus needs to be put on improving the curriculum to bring competency-based education, there are several ways that can help bring reform in the current medical education system. Some of these are;
- Leveraging technology to offer digital learning solutions
- Capitalizing on e-learning and facilitating infrastructure to support it
- Revising curriculum to have more practical training, competency-based skill development
- Inculcating problem-solving approach by situational/case-based examination
- A broad-based faculty development program to sharpen the competency of teachers
- Eliminating caste-based reservation and paving way for merit-based admission
- Industry academia collaboration to facilitate innovation
Way forward
- There should be a substantial step-up in public investment in medical education.
- By establishing new medical colleges, the government can increase student intake as well as enhance equitable access to medical education.
- Besides, it must allocate adequate financial resources to strengthen the overall capacity of existing medical colleges to enrich student learning and improve output.
Try this question for mains
Q. Considering the large diaspora of medical students across the globe do you consider there are problems in Indian medical education system? If there are any ,discuss them along with current health status and steps needed to counter them .
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Tamil Nadu NEET Exemption Bill sent to Home Ministry
From UPSC perspective, the following things are important :
Prelims level: NEET Quota row
Mains level: Read the attached story
The CM informed the Tamil Nadu Legislative Assembly that Governor has forwarded the NEET exemption Bill to the Union Home Ministry to be sent to the President of India for his assent.
What is the TN Bill about?
- The Bill exempts medical aspirants in Tamil Nadu from taking NEET examination for admission to UG degree courses in Indian medicine, dentistry and homeopathy.
- Instead, it seeks to provide admission to such courses on the basis of marks obtained in the qualifying examination, through “Normalization methods”.
- The aim of the Bill is to ensure “social justice, uphold equality and equal opportunity, protect all vulnerable student communities from being discriminated”.
- It seeks to bring vulnerable student communities to the “mainstream of medical and dental education and in turn ensure a robust public health care across the state, particularly the rural areas”.
Why TN is against NEET?
- Non-representative: TN opposes because NEET undermined the diverse societal representation in MBBS and higher medical studies.
- Disfavors the poor: It has favored mainly the affordable and affluent sections of the society and thwarting the dreams of underprivileged social groups.
- Exams for the elite: It considers NEET not a fair or equitable method of admission since it favored the rich and elite sections of society.
- Healthcare concerns: If continued, the rural and urban poor may not be able to pursue medical courses.
Can any state legislate against NEET?
- Admissions to medical courses are traceable to entry 25 of Concurrent List, Schedule VII of the Constitution.
- Therefore, the State can also enact a law regarding admission and amend any Central law on admission procedures.
Why is it going for President’s assent?
- The question is not whether the State government can amend a law falling under the Concurrent List.
- The question is whether the State government can exempt Section 10D of the IMC Act, which is a parliamentary law that falls under the Central List (Entry 66).
- Moreover, the Supreme Court has also upheld NEET as a requirement.
- Mere statistics highlighting that a majority of the stakeholders do not want NEET in Tamil Nadu is not an answer for exempting the examination.
Again, it is State and Centre are at crossroads
- Normally, a Bill requires assent from the Governor to become a law. Stalin’s contention is that this Bill deals with education, which is a Concurrent List subject.
- Admissions to medical courses fall under Entry 25 of List III, Schedule VII of the Constitution, and therefore the state is competent to regulate the same.
- Yet, as far as matters relating to the determination of standards for higher education are concerned, the central government has the power to amend a clause or repeal an Act.
- So, just the passing of the Bill doesn’t enable the students to get exempted from writing NEET.
- Already, Union Higher Education Secretary has held that if any State wants to opt out of the exam, it has to seek permission from the Supreme Court.
Options for Tamil Nadu
- Data is necessary only when there is power to legislate on the subject concerned.
- Since the Bill, which will become an Act only after the President’s nod, will come into effect only from the next academic year, the battle for and against the NEET requirement will continue in courts.
- Hopefully, the courts will determine the legality and have a definite solution to the question of medical admissions within the next year.
- Till such time, students who wrote NEET will fill the seats under the State quota.
Also read:
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Why do Indians go abroad for medical studies?
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: Medical education in India
- According to estimates from Ukraine, reported in the media, around 18,000 Indian students are in Ukraine (before Operation Ganga).
- Most of them are pursuing medicine.
- This war has turned the spotlight on something that has been the trend for about three decades now.
Preferred countries for medical degree
- For about three decades now, Indian students have been heading out to Russia, China, Ukraine, Kyrgyzstan, Kazakhstan, and Philippines to pursue a medical degree.
Hype of becoming a Doctor
- Prestige: The desire to study medicine still holds a lot of value in the Indian community (the other is becoming an IAS officer).
- Shortages of Doctor: In many rural areas, people still look at doctors as god’s incarnate.
- Rarity of opportunity: The lack of equal opportunities exacerbated by the caste factor in the Indian context, has a great deal of impact on the prestige still associated with being a doctor.
- Social upliftment ladder: For years, certain communities were denied the opportunities, and finally they do have a chance at achieving significant educational status.
Why go abroad?
- No language barrier: The medium of education for these students is English, a language they are comfortable with.
- Affordability: The amount spent on living and the medical degree are far more affordable than paying for an MBBS seat in private medical colleges in India.
- Aesthetics and foreign culture: People are willing to leave their home to study far away in much colder places and with completely alien cultures and food habits.
- Practice and OPD exposure: It broadens students’ mind and thinking, expose them to a whole range of experiences, and their approach to issues and crises is likely to be far better.
Doesn’t India have enough colleges?
(a) More aspirants than seats
- There are certainly far more MBBS aspirants than there are MBBS seats in India.
- In NEET 2021, as per a National Testing Agency press release, 16.1 lakh students registered for the exam, 15.4 lakh students appeared for the test, and 8.7 lakh students qualified.
- As per data from the National Medical Commission (NMC), in 2021-22, there were 596 medical colleges in the country with a total of 88,120 MBBS seats.
- While the skew is in favour of Government colleges, it is not greatly so, with the number of private medical institutions nearly neck-to-neck with the state-run ones.
(b) Fees structure
- That means over 50% of the total seats are available at affordable fees in Government colleges.
- Add the 50% seats in the private sector that the NMC has mandated must charge only the government college fees.
- In fully private colleges, the full course fees range from several lakhs to crores.
(c) Uneven distribution of colleges
- These colleges are also not distributed evenly across the country, with States such as Maharashtra, Karnataka, Tamil Nadu and Kerala having many more colleges.
What about costs?
- The cost factor on both sides of an MBBS degree is significant.
- The costs of an MBBS degree in a Government college tot up to a few lakhs of rupees for the full course, but in a private medical college, it can go up to ₹1 crore for the five-year course.
- In case it is a management seat, capitation fees can inflate the cost by several lakhs again.
- Whereas, an MBBS course at any foreign medical university in the east and Eastern Europe costs far less (upto ₹30lakh-₹40 lakh).
Way forward
- While PM Modi emphasised that more private medical colleges must be set up in the country to aid more people to take up MBBS, medical education experts have called for pause on the aspect.
- If the aim is to make medicine more accessible to students of the country, the path ahead is not in the private sector, but in the public sector, with the Central and State governments’ involvement.
- Starting private medical colleges by reducing the strict standards set for establishing institutes may not actually be the solution to this problem, if we think this is a concern.
Conclusion
- Creating more medical colleges will be beneficial for the country, if access and availability can be ensured.
- This will not be possible by resorting to private enterprise only.
- The State and Central governments can start more medical colleges, as recommended by NITI Aayog, by utilising district headquarters hospitals, and expanding the infrastructure.
- This way, students from the lower and middle socio-economic rung, who are otherwise not able to access medical seats, will also benefit.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Medical Ethics of Charaka
From UPSC perspective, the following things are important :
Prelims level: Charaka, Charaka Samhita, Ayurveda
Mains level: Medical Ethics of Charaka
The National Medical Commission (NMC), the regulator for medical education and practices that replaced the Medical Council of India in 2020, has suggested to medical colleges that the traditional Hippocratic Oath should be replaced by a “Charak Shapath”.
Who was Hippocrates?
- The Hippocratic Oath is attributed to Hippocrates of the island of Kos, a Greek physician of the classical period (4th-5th centuries BC, until the death of Alexander the Great in 323 BC).
- It broadly corresponds to the period from the death of the Buddha (486 BC) to the rise of the Mauryas (321 BC) in India.
- Among the great contemporaries of Hippocrates were the Athenian philosopher Plato and his teacher Socrates, and Plato’s student and Alexander’s tutor, the polymath Aristotle.
- He is regarded as the “father of modern medicine”.
What is the Hippocratic Oath?
- Basically, the Hippocratic Oath is a charter of ethical principles that physicians over the ages have sworn to uphold in the practice of their profession.
- The earliest available fragments of what is understood to be the original oath date back to the late 3rd century AD, and a millennium-old version is now in the library of the Holy See.
What are general outlines of a Medical Oath?
- Always exercise his/her independent professional judgment and maintain the highest standards of professional conduct
- Respect a competent patient’s right to accept or refuse treatment
- Not allow his/her judgment to be influenced by personal profit or unfair discrimination
- Be dedicated to providing competent medical service in full professional and moral independence, with compassion and respect for human dignity
- Deal honestly with patients and colleagues, and report to the appropriate authorities those physicians who practice unethically or incompetently or who engage in fraud or deception
- Certify only that which he/she has personally verified
- Respect the local and national codes of ethics
About Charaka and Charak Samhita
- The Charak Samhita is a medical pharmacopeia and collection of commentaries and discussions on medical practices that is dated to the 1st-2nd centuries AD.
- Along with the compendium of Susruta (c. 4th century AD), which is about surgery, the Charak Samhita is considered the foundational text of ancient Indian medicine,.
- It is an evolved system of understanding and treating disease that resembled that of Hippocrates and Galen (2nd century AD), and was in some ways ahead of the Greeks.
- In theory and praxis, ayurvedic medicine today remains broadly unchanged from these ancient Indian principles.
The medical ethics of Charaka
- The physician was an important and respected member of ancient Indian society, and medical practice followed rules of professional conduct and ethical principles. It goes on to say that-
- You must strive with all your soul for the health of the sick.
- You must not betray your patients, even at the cost of your own life.
- You must not get drunk, or commit evil, or have evil companions.
- You must be pleasant of speech…and thoughtful, always striving to improve your knowledge.
- When you go to the home of a patient you should direct your words, mind, intellect, and senses nowhere but to your patient and his treatment.
- Nothing that happens in the house of the sick man must be told outside, nor must the patient’s condition be told to anyone who might do harm by that knowledge to the patient or to another.
- This ethical code is universal, and remains just as relevant and applicable today.
Arguments in favour of Charaka Oath
- There is no universally accepted version of the physician’s oath.
- Many medical schools around the world hold a ceremony in which graduating doctors swear to a broad charter of ethics that are sometimes customised by individual institutions.
- A version of the ‘physician’s code of ethics’ is commonly displayed in hospitals or clinics in most places, including India.
Issues with this oath
- The opposition has criticised the proposal as an attempt to saffronise medical education.
- Introducing Indian elements into Indian education is necessary, but not at the expense of universal values and standards.
- Like several other sages mentioned in the literature of ancient India, the historicity of Charaka is still uncertain.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Legislative Powers of Governor
From UPSC perspective, the following things are important :
Prelims level: Legislative Powers of Governor
Mains level: Read the attached story
Tamil Nadu CM has charged that the Governor that he had failed to perform the duty vested in him by the Constitution when it came to deciding on the Bill adopted in the Legislative Assembly against the National Eligibility cum Entrance Test (NEET).
What is the issue?
- The Governor had returned the Bill to the Assembly Speaker instead of forwarding it for Presidential assent.
Constitutional Powers of the Governor
- Article 154: The executive power of the state shall be vested in the
governor and shall be exercised by him either directly or through
officers subordinate to him in accordance with this Constitution. - Article 163 (1): There shall be a council of ministers with the chief minister as the head to aid and advise the governor in the exercise of his functions, except in so far as he is required to exercise his functions in his discretion.
- Article 163 (2): If any question arises whether a matter falls within the governor’s discretion or not, the decision of the governor is final and the validity of anything done by him cannot be called in question on the ground that he ought or ought not to have acted in his discretion.
- The governor has constitutional discretion in the following cases:
a) Reservation of a bill for the consideration of the President (Articles 200 and 201).
b) Recommendation for the imposition of the President’s Rule in the state (Article 356).
c) While exercising his functions as the administrator of an adjoining Union territory (in case of an additional charge).
d) Special responsibility in 5th and 6th schedule areas.
e) Seeking information from the chief minister with regard to the administrative and legislative matters of the state. - Also, the governor has situational discretion (i.e., the hidden discretion derived from the exigencies of a prevailing political situation) in the following cases:
a) Appointment of the chief minister when no party has a clear-cut majority in the state legislative assembly or when the chief minister in office dies suddenly and there is no obvious successor.
b) Dismissal of the council of ministers when it cannot prove the confidence of the state legislative
assembly.
c) Dissolution of the state legislative assembly if the council of ministers has lost its majority.
What are the Legislative Powers of Governor?
Governor summons the sessions of both houses of the state legislature and prorogues them.
- The governor can even dissolve the State Legislative Assembly.
- These powers are formal and the governor’s use of these powers must comply with the advice of the Council of Ministers headed by the Chief Minister.
- He addresses the first session of the state legislature after the general elections in the state.
Appointments to the legislature
- He appoints 1/6th members of the State Legislative Council in states wherever there is a bicameral legislature.
- He nominates one member in the state legislative assembly from the Anglo-Indian Community if in view; the community is not well represented.
- Governor is empowered under Article 192 to disqualify a member of the State legislature when the election commission recommends that the legislator is no longer complying with provisions of Article 191.
Passing of Bills
- All the bills passed by the state legislatures are sent to the Governor for assent.
- Once a bill is sent to Governor for assent, he can:
a) Give assent to the bill
b) Withhold the assent
c) Return the bill to the legislature for reconsideration if it is not a money bill.
d) If the bill is re-passed by the legislature with or without amendment, the governor has to give assent to the bill.
e) Reserve the bill for consideration of the President.
When is the Bill sent to the President?
This is done under the circumstances when a bill:
- Violates the constitution or against directive principles of state policy (DPSP)
- Conflict with union powers
- Against the larger interest of the country and people
- May endanger the position of the high court in the state.
Ordinance making power
- When the state legislature is not in session and the governor considers it necessary to have a law, then the governor can promulgate ordinances.
- These ordinances are submitted to the state legislature at its next session.
- They remain valid for no more than six weeks from the date the state legislature is reconvened unless approved by it earlier.
Others
- As per Articles 165 and 177, Governor can ask the Advocate General to attend the proceedings of both houses of the state legislature and report to them any unlawful functioning if any.
Concerns with the role of governor
- Misuse of discretionary powers: States allege that this provision has often been misused by the governor who acts on the behest of the union government which is opposed to the basic scheme of the Indian Constitution.
- Appointment by centre: This often leads to the appointment of persons aligning with the party’s ideology to the post of Governor and he/she remains faithful to the Union government of the day rather than acting on the advice of the State Executive.
- Arbitrary removal: Even after Supreme Court Judgement in B.P. Singhal v. Union of India calling for a fixed tenure for Governors to encourage neutrality and fairness in the discharge of their duties, it is not being implemented on the ground.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Supreme Court upholds validity of OBC quota in NEET admissions
From UPSC perspective, the following things are important :
Prelims level: NEET Quota row
Mains level: Significance of the Judgment, New definition of Merit

The Supreme Court has pronounced its decision upholding the constitutional validity of providing 27% quota to Other Backward Classes (OBC) in NEET All India Quota (AIQ) seats for UG and PG medical courses.
What is the issue?
- The petitioners, several NEET aspirants, had argued that since the top court had limited reservation to 50% in the Indira Sawhney judgment, the government should have first applied to the court before tinkering with the quota calculations.
- The court further confirmed that there was no need for the Centre to have got the prior consent of the Supreme Court before introducing OBC quota in the AIQ seats under NEET.
- The court reasoned that material affluence of certain individual members of a socially backward group or ‘creamy layer’ could not be used against the entire group to deny it the benefits of reservation.
What is the background of this case?
- The government introduced OBC/EWS quota before the counselling of NEET counselling.
- The candidates applying for NEET PG were not provided any information on the distribution of the seat matrix.
- Such information is provided by the counselling authority only after the counselling session is to begin.
Key observations of the Apex Court
- The SC has held that reservation is not at odds with merit.
- It observed that ‘merit’ could not be narrowed to the limit of success in open competitive exams.
- Merit of a person is a sum total of “lived experiences” and his or her struggle to overcome cultural and social setbacks, observed the SC.
Why is this a landmark judgment?
- Merit cannot be reduced to narrow definitions of performance in an open competitive examination, which only provides formal equality of opportunities , said the SC.
- Current competencies are assessed by competent examinations but are not reflective of excellence, capability and potential of an individual.
Major justifications for Reservations
- Exams did not reflect how social, economic and cultural advantages that accrued to certain classes contributed to their success in them, the court noted.
- Examinations are not a proxy for merit.
- Merit should be socially contextualized and re-conceptualized.
- Reservation is not at odds with merit but furthers its distributive impact, Justice Chandrachud observed.
Constitutionality of the decision
- The court held that the power of the State governments to provide reservations under Article 15 (4) and (5) of the Constitution was not an “exception” to Article 15 (1).
- It enshrines the mandate that “the State shall not discriminate against any citizen on grounds only of religion, race, caste, sex, and place of birth or any of them”.
- The court held that the power of the State government to craft reservations for the OBC amplified the principle of “substantive equality” manifested through Article 15 (1).
Implications: Victory for States
- In a significant victory for States such as Tamil Nadu, the court confirmed their power to make “special provisions” and provide reservations in educational admissions, whether in aided or unaided institutions.
- TN provides government jobs for the advancement of “any socially and educationally backward classes of citizens or for the SCs and STs”.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
NEET hasn’t created the equality of opportunity
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2- Issues with NEET
Context
The Tamil Nadu government has passed an Act seeking an exemption from treating NEET as the sole and mandatory requirement for medical admission in the state. The Act, which is yet to get approval from the President.
NEET issue in Tamil Nadu
- The Justice A K Rajan committee was appointed by the state government of Tamil Nadu to examine whether NEET is an equitable method of selection.
- Its report lends credence to the belief that NEET tends to give an advantage to students from privileged backgrounds.
- It also observed that NEET, in terms of orientation, is biased towards the Central Board of Secondary Education (CBSE).
- In the section titled ‘Size of coaching market’, the report brings out two poignant facts.
- One, by inadvertently creating a “market for coaching”, NEET has helped to create an “extractive industry of coaching” as an essential condition for clearing it.
- Two, the coaching fees are not only high, but are beyond the reach of many, especially the poor and marginalised.
- Acting upon the committee’s recommendation, the Tamil Nadu government has passed an Act seeking an exemption from treating NEET.
- The Act, which is yet to get approval from the President.
- An educational intervention which was introduced as a solution to foster equality of opportunity has turned out to be the primary cause of deepening inequality of participation and opportunity.
Important questions
- There are at least two important questions.
- Equality of opportunity: First, does NEET help foster equality of opportunity for everyone without unduly advantaging or disadvantaging anyone?
- Second, is NEET’s bias towards CBSE justifiable in an immensely diverse country like ours, where varied school curricula coexist with a highly unequal access to financial and educational resources and opportunities?
- The question here is: How can NEET promote parity of participation when aspiring first-generation students from marginalised and poor households participate from a highly unequal position in the first place?
- NEET disregards the fact that the terms and conditions of participation are highly unequal and biased.
Way forward
- The National Education Policy (NEP 2020) envisions a curriculum and pedagogy which will promote holistic learning, social responsibility and multilingualism, among other things.
- It is important, therefore, to significantly restructure the focus of NEET keeping in mind the spirit of NEP and varied school curricula in regional languages.
Conclusion
A restructured NEET, which does not require intensive and repeated coaching as a prerequisite and is not biased towards any board, can go a long way in promoting the parity of participation and nourishing the capacity to aspire, especially of the poor and marginalised.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
NITI Aayog’s proposal of allowing private entities to take over district hospitals
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2- Reforming medical education in India
The article highlights the issue of shortage of doctors in India and issues with the involvement of private sector in it.
Government approach
- Market-oriented approach towards medical education: NITI Aayog’s proposal of allowing private entities to take over district hospitals for converting them into teaching hospitals with at least 150 MBBS seats.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Standards must not be lowered to certify Ayurveda postgraduates surgeons
From UPSC perspective, the following things are important :
Prelims level: Sushrut Samhita
Mains level: Debate over mixopathy
This conundrum of different standards for surgical training must be solved because patient safety is far more important than the career progression of Ayurvedic postgraduates.
Practice Question: There is a need to rethink on the recent notification of AYUSH Ministry allowing Ayurveda postgraduates to conduct surgeries keeping the safety of the patient at the centre. Discuss.
The current clash
- The clash between the allopathic and AYUSH fraternities is about the AYUSH practitioners’ “right” to conduct surgeries.
- The Ayurvedic fraternity maintains postgraduates in Shalya and Shalakya (two surgical streams among 14 post-graduate courses) are taught procedures listed in the curriculum.
- The oldest-known surgical specialist was, in fact, an Ayurvedic surgeon/sage Sushrut (600 BC) who wrote the Sushrut Samhita — a profound exposition on conducting human surgery which continues to receive worldwide acclaim.
- Surgery was practised by Ayurvedic surgeons long before the advent of western medicine.
- Allopaths question the logic of Sushrut’s millennia-old pre-eminence bestowing the right to practise modern surgery. Ayurvedic surgeons may not know the hidden risks of every surgical procedure and how to surmount sudden mishaps.
- The Ministry of AYUSH justifies its notification on the ground that not all vaidyas but only postgraduates qualifying from two surgical streams have been authorized to perform selected surgeries.
The contentious issue
- The moot point is about who decides whether Ayurvedic surgeons possess sufficient proficiency to conduct these surgeries safely and by what standard their skills are judged.
- Surgical proficiency cannot be judged by different standards in one country — particularly when less-educated patients would rather save money than question a surgeon’s qualifications.
- The statutory regulatory body for AYUSH education is the Central Council of Indian Medicine (CCIM). CCIM has only promoted what private college managements demand, propelled, in turn, by students’ need to earn a stable income as medical professionals.
- In this misplaced zeal to give better earnings to the Ayurvedic vaidyas, CCIM has sidelined many skills that Ayurveda could have included, which are relevant even today.
- This has subjugated the curriculum to nurture more and more replicas of doctors of modern medicine.
- This has killed the knowledge, purity and goodness of classical Ayurveda, which ironically is the Ayurveda in high demand in Europe, Russia and America.
Nothing can replace practise and training to perform surgery
- When it comes to surgery, it is not knowledge but rigorous training and continuous practice which makes for perfection. Both require clinical material and most Ayurvedic hospitals do not have a fraction of the surgical patients found in allopathic general hospitals.
- Allopathic students of surgery learn first by watching and then performing scores of surgeries under supervision.
- Surgical skills are by no means impossible to learn but they become difficult to master without continuous training and supervision.
- Due to the paucity of patients, limited scope for training and access to gaining hands-on practice, it is hazardous to allow all Shalya and Shalakya postgraduates to undertake surgical procedures.
- In the last three decades, specialization has excluded general surgeons from performing what was once considered routine. For example, only an ENT surgeon can perform a tonsillectomy.
- Therefore, to notify that Ayurvedic postgraduates in surgery can perform omnibus operations runs counter to the norm in India and in other countries.
Way forward
- In performing surgery, the only benchmark should be the duration of hands-on training received — counted by surgeries under supervision, and being judged through external evaluation.
- Every surgeon’s skills and competence must be tested by applying exactly the same standards before she/he can operate.
- This conundrum of different standards for surgical training must be solved because patient safety is far more important than the career progression of Ayurvedic postgraduates.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Issues related to Nursing Sector in India
From UPSC perspective, the following things are important :
Prelims level: Not Much
Mains level: Nursing education in India
The year 2020 has been designated as “International Year of the Nurse and the Midwife”.
But the nursing education in India displays a grim situation. It suffers poor quality of training, inequitable distribution, and non-standardized practices.
Nursing sector in India
- Nurses and midwives will be central to achieving universal health coverage in India.
- India’s nursing workforce is about two-thirds of its health workforce. Its ratio of 7 nurses per 1,000 population is 43% less than the World Health Organization norm; it needs 2.4 million nurses to meet the norm.
- The sector is dogged by structural challenges that lead to poor quality of training, inequitable distribution, and non-standardized practices.
Uneven regulation
Nursing education in India has a wide array of certificate, diploma, and degree programmes for clinical and non-clinical nursing roles.
- The Indian Nursing Council regulates nursing education through prescription, inspection, examination, and certification. 91% of the nursing education institutions are private and weakly regulated. The quality of training of nurses is diminished by the uneven and weak regulation.
- The current nursing education is outdated and fails to cater to the practice needs. The education, including re-training, is not linked to the roles and their career progression in the nursing practice.
- There are insufficient postgraduate courses to develop skills in specialities and address critical faculty shortages both in terms of quality and quantity.
- These factors have led to gaps in skills and competencies, with no clear career trajectory for nurses.
- Multiple entries point to the nursing courses and lack of integration of the diploma and degree courses diminish the quality of training.
- A common entrance exam, a national licence exit exam for entry into practice, and periodic renewal of licence linked with continuing nursing education would significantly streamline and strengthen nursing education.
- Transparent accreditation, benchmarking, and ranking of nursing institutions too would improve the quality.
- The number of nursing education institutions has been increasing steadily but there are vast inequities in their distribution. Around 62% of them are situated in southern India.
- There is little demand for postgraduate courses. Recognizing the need for speciality courses in clinical nursing 12 PG diploma courses were rolled out but the higher education qualification is not recognized by the recruiters.
- The faculty positions vacant in nursing college and schools are around 86% and 80%, respectively.
Gaps in education, services
- There is a lack of job differentiation between diploma, graduate, and postgraduate nurses regarding their pay, parity, and promotion.
- The higher qualifications are underutilized, leading to low demand for postgraduate courses.
- Those with advanced degrees seek employment in educational institutions or migrate abroad which has led to an acute dearth of qualified nurses in the country.
- Small private institutions with less than 50 beds recruit candidates without formal nursing education. They are offered courses of three to six months for non-clinical ancillary nursing roles and are paid very little.
- The Indian Nursing Act primarily revolves around nursing education and does not provide any policy guidance about the roles and responsibilities of nurses in various cadres.
- Nurses in India have no guidelines on the scope of their practice and have no prescribed standards of care and is a major reason for the low legitimacy of the nursing practice and the profession. This may endanger patient safety.
- The Consumer Protection Act holds only the doctor and the hospital liable for medico-legal issues; nurses are out of the purview of the Act. This is contrary to the practices in developed countries where nurses are legally liable for errors in their work.
Institutional reforms required
- The governance of nursing education and practice must be clarified and made current.
- The Indian Nursing Council Act of 1947must be amended to explicitly state clear norms for service and patient care, fix the nurse to patient ratio, staffing norms and salaries.
- The jurisdictions of the Indian Nursing Council and the State nursing councils must be explained and coordinated so that they are synergistic.
- Incentives to pursue advanced degrees to match their qualification, clear career paths, the opportunity for leadership roles, and improvements in the status of nursing as a profession should be done.
- A live registry of nurses, positions, and opportunities should be a top priority to tackle the demand-supply gap in this sector.
- The public-private partnership between private nursing schools/colleges and public health facilities is another strategy to enhance nursing education. NITI Aayog has recently formulated a framework to develop a model agreement for nursing education.
- The Government has also announced supporting such projects through a Viability Gap Funding.
Practice Question:
Q. Discuss the various issues related to nursing sector in India and measures to be taken to address them.
A Bill that could spell hope
- The disabling environment prevalent in the system has led to the low status of nurses in the hierarchy of health-care professionals. In fact, nursing has lost the appeal as a career option.
- The National Nursing and Midwifery Commission Bill currently under consideration should hopefully address some of the issues highlighted.
- These disruptions are more relevant than ever in the face of the COVID-19 pandemic.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Surgery as part of Ayurveda
From UPSC perspective, the following things are important :
Prelims level: Sushrut Samhita
Mains level: Read the attached story
Last month, a government notification listed out specific surgical procedures that a postgraduate medical student of Ayurveda must be “practically trained to acquaint with, as well as to independently perform”.
Q.Allowing modern surgeries to Ayurveda professionals is a mixopathy and an encroachment into the jurisdiction and competencies of modern medicine. Critically analyse.
What is the notification?
- The notification mentions 58 surgical procedures that postgraduate students must train themselves in and acquires skills to perform independently.
- These include procedures in general surgery, urology, surgical gastroenterology, and ophthalmology.
The issue
- The notification has invited sharp criticism from the Indian Medical Association, which questioned the competence of Ayurveda practitioners to carry out these procedures.
- They have called the notification as an attempt at “mixopathy”.
- The IMA has planned nationwide protests against this notification and has threatened to withdraw all non-essential and non-Covid services.
Surgery as a part of Ayurveda
- It is not that Ayurveda practitioners are not trained in surgeries, or do not perform them.
- In fact, they take pride in the fact that their methods and practices trace their origins to Sushruta, an ancient Indian sage and physician.
- The comprehensive medical treatise Sushruta Samhita has, apart from descriptions of illnesses and cures, detailed accounts of surgical procedures and instruments.
- There are two branches of surgery in Ayurveda — Shalya Tantra, which refers to general surgery, and Shalakya Tantra which pertains to surgeries related to the eyes, ears, nose, throat and teeth.
- All postgraduate students of Ayurveda have to study these courses, and some go on to specialize in these and become Ayurveda surgeons.
Distinctions in surgical procedures
- For several surgeries Ayurvedic procedures almost exactly match those of modern medicine about how or where to make a cut or incision, and how to perform the operation.
- There are significant divergences in post-operative care, however.
- The only thing that Ayurveda does not do is super-speciality surgeries, like neurosurgery or open-heart surgeries.
- For most other needs, there are surgical procedures in Ayurveda. It is not very different from allopathic medicine.
Ayurvedic surgeries before the notification
- PG education in Ayurveda is guided by the Indian Medical Central Council (Post Graduate Education) Regulations framed from time to time.
- Currently, the regulations formulated in 2016 are in force. The latest notification of last month is an amendment to the 2016 regulations.
- The 2016 regulations allow postgraduate students to specialise in Shalya Tantra, Shalakya Tantra, and Prasuti evam Stree Roga (Obstetrics and Gynecology), the three disciplines involving major surgical interventions.
- Students of these three disciplines are granted MS (Master in Surgery in Ayurveda) degrees.
Arguments in favour
- Ayurveda practitioners point out that students enrolling in Ayurveda courses have to pass the same NEET (National Eligibility-cum-Entrance Test).
- Ayurveda institutions prescribe textbooks from modern medicine, or that they carry out surgeries with the help of practitioners of modern medicine.
- Their course, internship and practice also run parallel to the MBBS courses.
- Postgraduate courses require another three years of study. They also have to undergo clinical postings in the outpatient and In-patient departments at hospitals apart from getting hands-on training.
- Medico-legal issues, surgical ethics and informed consent is also part of the course apart from teaching Sushruta’s surgical principles and practices.
So, what is new?
- Ayurveda practitioners say the latest notification just brings clarity to the skills that an Ayurveda practitioner possesses.
- The surgeries that have been mentioned in the notification are all that are already part of the Ayurveda course. But there is little awareness about these.
- A patient is usually not clear whether an Ayurvedic practitioner has the necessary skill to perform one of these operations.
- Now, they know exactly what an Ayurveda doctor is capable of. The skill sets have been defined. This will remove question marks on the ability of an Ayurveda practitioner.
What are the IMA’s objections?
- IMA doctors insist that they are not opposed to the practitioners of the ancient system of medicine.
- But they say the new notification somehow gives the impression that the skills or training of the Ayurveda doctor in performing modern surgeries are the same as those practising modern medicine.
- This, they say, is misleading, and an “encroachment into the jurisdiction and competencies of modern medicine”.
- The IMA has condemned the move calling it predatory poaching on modern medicine and its surgical disciplines.
- The IMA has demanded that the notification, as well as the NITI Aayog, move towards ‘One Nation One System’ (of AYUSH) be withdrawn.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
Dealing with the problems of medical education
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2- Issues with medical education in India
The article discusses the issues with medical education in India and how it affects the principle of equality.
Role of private entities
- Due to demand for high-quality medical care on the one hand and constraints on public resources on the other, private entities have been permitted to establish medical educational institutions to supplement government efforts.
- In the field of health care, there is a continuing shortage of health-care personnel.
- The infrastructure required for high-quality modern medical education is expensive.
- The three stated objectives of medical education has been — providing health-care personnel in all parts of the country, ensuring quality and improving equity.
- None of the three stated objectives of medical education has been achieved by the private sector.
- Though they are supposed to be not-for-profit, taking advantage of the poor regulatory apparatus and the ability to both tweak and create rules, these private entities, with very few exceptions, completely commercialised education.
Demand for regulation and equity
- There have been attempts to regulate fees, sometimes by governments and sometimes by courts.
- These efforts have not been fruitful.
- The executive, primarily the Medical Council of India, has proven unequal to the task of ensuring that private institutions comply with regulations.
- When the courts are approached, which issues are seen as important depends on the Bench.
- It was in this situation that led to the introduction of the National Eligibility-cum-Entrance Test (Undergraduate), or NEET-UG, as a single all-India gateway for admission to medical colleges.
- Challenged in courts, after an initial setback, the NEET scheme has been upheld.
How NEET affected equity
- NEET may have improved the quality of candidates admitted to private institutions to some extent, but it seems to have further worsened equity.
- Under any scheme of admission, the number of students from government schools who are able to get admission to a medical college is very low.
- With NEET, the number has become lower.
- The high fees of private medical colleges have always been an impossible hurdle for students from government schools, whatever the method used for admission.
Way forward
- The basic cause of inequity in admission to higher educational institutions is the absence of a high quality school system accessible to all.
- Allowing government medical colleges to admit students based on marks in Standard XII and using NEET scores for admission to private colleges will be more equitable right now.
Conclusion
Only a resolute government, determined to ensure that economic policy facilitates quality and equity in education, can do it.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Medical Education Governance in India
National Medical Commission
From UPSC perspective, the following things are important :
Prelims level: National Medical Commission
Mains level: Not Much
The National Medical Commission (NMC) has replaced the Medical Council of India (BoG-MCI), as per information released by the Health Ministry.
National Medical Commission
- National Medical Commission (NMC) is an Indian regulatory body of 33 members which regulates medical education and medical professionals.
- It replaced the Medical Council of India (MCI) on 25 September 2020.
- The Commission grants recognition of medical qualifications, gives accreditation to medical schools, grants registration to medical practitioners, and monitors medical practice and assess the medical infrastructure in India.
- The NMC will have four separate autonomous boards: under-graduate medical education, post-graduate medical education, medical assessment and rating and ethics and medical registration.
It’s legal backing
- The NITI Aayog had recommended the replacement of MCI with NMC.
- The decision was approved by most states and after its approval by the Prime Minister and NMC bill was passed by parliament and approved by President on 8 August 2019.
- National Medical Commission ordinance was brought in to replace Medical Council of India in early 2019 through an ordinance issued in January 2019 by the President of India.
- The Supreme Court had allowed the Central Government to replace the medical council and with the help of five specialized doctors monitor the medical education system in India, from July 2017.
- The government dissolved the MCI in 2018 and Indian Medical Council Act, 1956 (102 of 1956) stands repealed.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
The MCI has been in the news for the wrong reasons as the Parliamentary Standing Committee on Health in its 92nd report came down heavily on various aspects of the functioning of MCI. British medical Journal also had suggested radical revamp of the MCI. This articles focuses on the medical education governance in India.
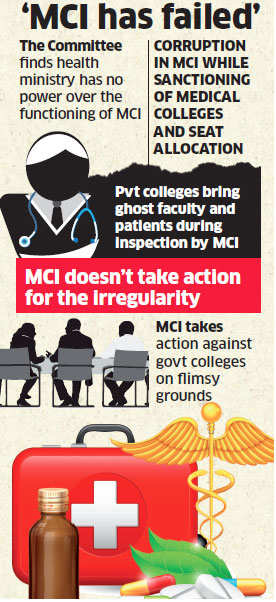
source
Let’s understand the issues under the following heads:
- Context
- Background
- Weaknesses Highlighted by Parliamentary panel
- What are the major reforms needed in MCI?
- Measures needed to overhaul and revamp MCI
- Mandate of Lodha committee
- Way forward
Context:
- MCI has been criticised for being a ‘biased’ organisation, acting ‘against larger public health goals’ and an ‘exclusive club’ of medical doctors from corporate hospitals and private practice. The British Medical Journal (BMJ) and the Parliamentary Standing Committee in their recent report have called for a ‘radical prescription’ to reform the Medical Council of India (MCI) in order to eliminate corruption and lack of ethics in healthcare.
- SC appointed a three-member committee headed by former Chief Justice of India R M Lodha to oversee MCI.
Background
- The MCI was established under the Indian Medical Council Act 1933 and given responsibility for maintaining standards of medical education, providing ethical oversight, maintaining the medical register, and, through amendments in 1993, sanctioning medical colleges has failed to deliver quality and integrity in the health services across India.
- The Medical Council of India (MCI) is a statutory body entrusted with the responsibility of establishing and maintaining high standards of medical education in India.
Weaknesses Highlighted by Parliamentary panel
In its scathing report, the standing committee felt that the MCI has repeatedly failed on all its mandates over the years. The committee noted the following as some of the prominent failures of MCI.
- Failure to create a curriculum that produces doctors suited to working in Indian context especially in the rural health services and poor urban areas. The committee felt that this has created disconnect between medical education system and health system.
- Failure to maintain uniform standards of medical education, both at the undergraduate and post-graduate levels.
- Devaluation of merit in admission, particularly in private medical institutions due to prevalence of capitation fees, which make medical education available only to the rich and not necessarily to the most deserving.
- Non-involvement of the MCI in any standardized summative evaluation of the medical graduates and post-graduates.
- Failure to put in place a robust quality assurance mechanism.
- Very little oversight of PG medical education leading to huge variation in standards.
- Failure to create a transparent system of medical college inspections and grant of recognition or de-recognition.
- Failure to oversee and guide the Continuing Medical Education in the country, leaving this important task in the hands of the commercial private industry.
- Failure to instill respect for a professional code of ethics in the medical professionals and take disciplinary action against doctors found violating the code of Ethics.
What are the major reforms needed in MCI?
- There is a need to restructure the MCI. It should not be an elected body dominated by vested interest but should represent all stakeholders through nomination. The MCI, as presently elected, neither represents professional excellence nor its ethos. The current composition of the Council reflects that more than half of the members are either from 21 corporate hospitals or in private practice.
- The MCI currently sets standards for recognition, inspects and licenses medical colleges; overseas Registration and Ethical Conduct of Doctors. It now proposes to undertake accreditation as well. Such concentration of powers creates a serious conflict of interest and provides a fertile ground for misuse of authority. So there is a need to create a transparent system of licensing of medical colleges.
- There should be bifurcation of the functions of MCI and recommends that different structures be created for discharging different functions.
- There is a need to revisit ICT tools and revisit minimum standards which are required under the act to establish medical colleges.
- A code of ethics which is in line with the international standards needs to be developed for the medical professionals to reduce the corrupt practices.
- It needs to see a balance between the number of seats available for medical courses at undergraduate and postgraduate level.
Measures needed to overhaul and revamp MCI
- The Parliamentary committee made a number of recommendations to overhaul the system. Some of the important recommendations of the committee are the following,
- Doctor – Population ratio in India is 1:1674 as against the WHO norm of 1:1000, hence the government should immediately spell out policy stance in great detail to augment the capacity of production of doctors including specialists and super-specialists at the scale and speed required to meet India’s health needs.
- The regulatory framework of medical education and practice should be comprised of professionals of the highest standards of repute and integrity, appointed through a rigorous and independent selection process.
- Urgent measures have to be taken to restructure the composition of MCI to encourage diversity so that it does not become an exclusive club of doctors.
- Physical infrastructure requirement should be pruned down in such a way that it should have just about 30 to 40 percent standing value in the total assessment of a medical college.
- Support to convert district hospitals into medical colleges. If a district hospital is converted into a medical college, it will not only be equipped with specialists of all disciplines, providing the healthcare services across the whole spectrum but will also produce some doctors in its area of operation and will thus help reduce geographical mal-distribution of doctors.
- The PG entrance exam should be held immediately after the final MBBS examination so that the graduate doctor could concentrate on practical skills during his internship.
- Ethics should be made one of the cornerstones of the syllabus of medical education.
- Introduction of Common Medical Entrance Test (CMET) should be done across the nation barring those States who wish to remain outside the ambit of the CMET. A common exit test should be introduced for MBBS doctors.
Mandate of the Lodha committee
- Lodha Committee would have complete authority to oversee all statutory functions under the MCI Act.
- All policy decisions of the MCI will need approvals from the Committee. It will also be free to issue remedial directions.
- The Committee will function for 1 year, unless a suitable mechanism is brought in earlier by it.
- Initially the panel will function for a year, unless suitable mechanism is brought in place earlier which will substitute the said committee.
Way forward
- The abysmal doctor-patient ratios in India’s rural areas and poorer districts, the sanctioning of new medical colleges without ensuring trained medical faculty, the failure to produce adequate specialist doctors, and corruption in the conduct of inspections and in granting sanctions to medical colleges have wrecked the MCI’s credibility.So, there is a need to bring back the integrity which MCI has lost over the years.
- Whether Lodha Committee manages to inculcate the changes needed in MCI or ends up being one of the numerous other attempts at cleaning up the medical education scene remains to be seen.
References: