Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Vaccinating India: On Zero-Dose Children
Why in the News?
India has made significant progress in expanding vaccine coverage, with a dramatic drop in the percentage of zero-dose children from 33.4% in 1992 to 6.2% in 2023. But even though India is not affected by war or extreme poverty like some other countries, it still has the second-highest number of children without any vaccination in the world.
What is the trend in global and Indian vaccine coverage?
|
What are zero-dose children?
- Zero-dose children are those who have not received the first dose of the diphtheria, tetanus, and pertussis (DTP) vaccine.
- They are a crucial performance marker of a country’s immunisation system and indicate inequities in vaccine coverage.
Why are they important for assessing vaccination?
- Reflects health system coverage and equity: A high number of zero-dose children shows that vaccination programmes are not reaching all segments of the population. NFHS-5 (2019–21) Data also showed that full immunisation coverage among children aged 12–23 months was significantly lower in rural and tribal regions compared to urban areas (e.g., Nagaland: 57.8%, compared to Tamil Nadu: 89.8%).
- Indicates social and economic exclusion: The presence of zero-dose children highlights barriers like poverty, low maternal education, and marginalisation. Eg: Urban slums with high migrant populations tend to have more zero-dose children due to lack of awareness and access.
- Warns of vulnerability to disease outbreaks: Areas with many zero-dose children are more likely to face outbreaks of vaccine-preventable diseases. Eg: Measles outbreaks are more common in districts with poor immunisation coverage.
Why does India still have a high number of zero-dose children despite adequate resources?
- High birth rate increases absolute numbers: India has the highest number of annual births globally. In 2023, India had around 23 million births, making even a small percentage of zero-dose children translate into a large number.
- Geographical and logistical challenges: Remote tribal areas, urban slums, and migrant populations are harder to reach due to terrain, mobility, and poor infrastructure. E.g., children in parts of Meghalaya or urban Delhi, slums often miss vaccinations due to lack of access and follow-up.
- Socio-cultural barriers and vaccine hesitancy: Low maternal education, religious beliefs, and misinformation lead to vaccine hesitancy in certain communities. Eg: In some Muslim households or among Scheduled Tribes, distrust or misinformation about vaccines limits uptake.
How has India’s zero-dose child rate changed over time, especially post-COVID?
- Steady decline before the pandemic: Between 1992 and 2016, India reduced the percentage of zero-dose children from 33.4% to 10.1%, showing consistent improvement in immunisation outreach.
- Sharp rise during the COVID-19 pandemic: Disruptions in health services led to a surge in zero-dose children, increasing from 1.4 million in 2019 to 2.7 million in 2021, reversing years of progress.
- Partial recovery after the pandemic: The number dropped to 1.1 million in 2022 but rose again to 1.44 million in 2023, indicating ongoing challenges in sustaining immunisation coverage.
Where are zero-dose children mainly located in India?
- High-burden states in northern and central India: Large numbers of zero-dose children are concentrated in Uttar Pradesh, Bihar, Maharashtra, Rajasthan, Madhya Pradesh, and Gujarat, which have large populations and gaps in last-mile immunisation delivery.
- Northeastern and underserved regions: A relatively high proportion is also found in Meghalaya, Nagaland, Mizoram, and Arunachal Pradesh, where geographic inaccessibility, scattered populations, and weaker health infrastructure pose challenges.
What actions are needed for India to meet the WHO’s 2030 immunisation target?
- Expand and intensify targeted immunisation drives: Strengthen last-mile delivery through regular and focused vaccination campaigns in underserved regions. Eg: Mission Indradhanush and its intensified versions could increase immunisation coverage in low-performing districts.
- Strengthen community-level engagement and awareness: Promote behavioural change and reduce vaccine hesitancy through culturally tailored IEC (Information, Education, and Communication) activities. Eg: Janani Suraksha Yojana (JSY) encourages institutional deliveries and postnatal care, which can be used to ensure timely vaccination of newborns.
- Integrate immunisation with digital health monitoring systems: Use technology for real-time tracking of vaccine coverage and follow-up in high-birth and high-risk areas. Eg: eVIN (Electronic Vaccine Intelligence Network) monitors vaccine stocks and cold chain availability, improving efficiency and reducing wastage.
Conclusion: India’s immunisation journey shows a mixed reality, while the country is a global leader in vaccine development, it still struggles to ensure all its children receive basic immunisation. Closing this gap is important not just for public health but also for social fairness and overall development. The need is even more urgent because India has the highest number of newborns in the world. The Immunisation Agenda 2030 should be treated as a national priority.
Mains PYQ:
[UPSC 2022] How do vaccines work? What approaches were adopted by the Indian vaccine manufacturers to produce COVID-19 vaccines?
Linkage: It explicitly deals with “vaccines” and “Indian vaccine manufacturers”. While it focuses on COVID-19 vaccines, the discussion around vaccine functionality and production capacity is fundamentally linked to the broader challenge of “Vaccinating India” and reaching “zero-dose children” for various preventable diseases.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
National Polio Surveillance Network (NPSN)
Why in the News?
The Indian government has proposed a phased winding down of the National Polio Surveillance Network (NPSN), a WHO-established network critical to tracking and eliminating polio in India.
About National Polio Surveillance Network (NPSN):
- Launch : The NPSN was established in 1997 as a collaboration between the World Health Organization (WHO) and the Ministry of Health and Family Welfare (MoHFW), Government of India.
- Objective: Its main goal is to detect and monitor the poliovirus in India to enable quick response and containment.
- Operational Structure: The network functions under the National Polio Surveillance Project (NPSP) and includes over 200 field surveillance units across the country.
- Methodology: The core method is Acute Flaccid Paralysis (AFP) surveillance, which tracks sudden paralysis in children under 15 — a key indicator of polio.
- Environmental Surveillance: The NPSN also tests sewage and water samples to detect silent circulation of the virus.
- Laboratory Support: A network of WHO-accredited laboratories confirms virus presence through testing of stool and water samples.
- Rapid Response: Every suspected case is quickly investigated, and public health teams are deployed for control and containment.
- Expanded Role: Over time, NPSN has also supported surveillance for measles, rubella, DPT, and helped train health workers on new vaccines.
Polio and Its Eradication in India:
- About: Polio is a highly infectious viral disease primarily affecting children under 5, potentially causing paralysis or death.
- Transmission: The disease spreads via the faecal-oral route, mostly through contaminated water or food.
- Types of Polioviruses:
- WPV1 still exists in Pakistan and Afghanistan.
- WPV2 and WPV3 have been eradicated globally.
- Infection Mechanism: Once inside the body, the virus multiplies in the intestines and may attack the nervous system, causing permanent paralysis.
- Prevention through Vaccination:
- Oral Polio Vaccine (OPV) is given at birth, 6, 10, and 14 weeks, with a booster at 16–24 months.
- Injectable Polio Vaccine (IPV) is administered with the third DPT dose under the Universal Immunization Programme (UIP).
- Pulse Polio Campaign (1995): India launched the Pulse Polio Immunization Campaign, providing oral polio drops to all children under 5.
- Eradication Milestones: The last wild polio case in India was reported in 2011, and in 2014, WHO officially declared India polio-free.
- Role of NPSN: The success was enabled by strong surveillance, mass immunization, and dedicated work by NPSN and its partners.
| [UPSC 2016] ‘Mission Indradhanush’ launched by the Government of India pertains to:
(a) Immunization of children and pregnant women* (b) Construction of smart cities across the country (c) India’s own search for the Earth-like planets in outer space (d) New Educational Policy |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
India’s first ICMR-SCD Stigma Scale
Why in the News?
The Indian Council of Medical Research (ICMR) has developed the ICMR-SCD Stigma Scale for India (ISSSI) to help understand and reduce stigma faced by patients and caregivers from sickle cell disease (SCD).
What is Sickle Cell Disease (SCD)?
|
About the ICMR-SCD Stigma Scale for India (ISSSI):
- Purpose: The ISSSI is India’s first tool designed to measure stigma faced by sickle cell disease (SCD) patients and their caregivers.
- Developing Authority: It was developed by ICMR to understand and address the social impact of SCD in India’s diverse communities.
- Global Context: This is the fourth stigma scale worldwide and the first validated for Indian conditions.
- Scientific Validation: The tool was validated in a study published in The Lancet (Regional Health – South-East Asia).
- Availability: The ISSSI is now approved for use in both clinical and research settings across India.
- Components: It includes two formats — ISSSI-Pt for patients and ISSSI-Cg for caregivers.
- Stigma Dimensions: It captures issues related to family expectations, reproductive concerns, social disclosure, illness burden, interpersonal challenges, and negative healthcare experiences.
- Data Sources: The scale was developed using inputs from 6 culturally diverse districts: Alluri Seetharama Raju, Anuppur, Chhoteudepur, Kandhamal, Mysuru, and Udalguri.
India’s Strategy: Anaemia Mukt Bharat (AMB)
- Launch Year: The AMB Mission was launched in 2018 to reduce anemia using a 6x6x6 strategy.
- Target Groups: It covers six groups — young children, school children, adolescents, women of reproductive age, pregnant women, and lactating mothers.
- Key Interventions: Actions include iron and folic acid supplements, deworming, nutrition education, digital health tools, IFA-fortified foods, and disease screening (including SCD).
- Supporting Systems: It is backed by inter-ministerial coordination, state-level units, research centers, the AMB Dashboard, digital tracking, and supply chain support.
- Reach: The mission aims to impact around 450 million people, focusing on real-time monitoring and last-mile delivery.
| [UPSC 2023] Consider the following statements in the context of interventions being undertaken under Anaemia Mukt Bharat Strategy:
1. It provides prophylactic calcium supplementation for pre-school children, adolescents and pregnant women. 2. It runs a campaign for delayed cord clamping at the time of child-birth. 3. It provides for periodic deworming to children and adolescents. 4. It addresses non-nutritinoal causes of anaemia in endemic pockets with special focus on malaria, hemoglobinopathies and fluorosis. How many of the statements given above are correct? Options: (a) Only one (b) Only two (c) Only three* (d) All four |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[17th May 2025] The Hindu Op-ed: The ingredient to turn around nutrition outcomes
PYQ Relevance:[UPSC 2024] Distinguish between gender equality, gender equity and women’s empowerment. Why is it important to take gender concerns into account in programme design and implementation? Linkage: Gender concerns are important in programme design, aligning with the article’s argument that nutrition programmes like POSHAN have limited impact. |
Mentor’s Comment: India’s free foodgrain programme, which supports 800 million people, shows a harsh truth: hunger and malnutrition are still big problems. In this fight against malnutrition, women and girls are often ignored. Even though the economy is growing and many welfare schemes exist, nutrition is still very unequal, especially for women. The government started the POSHAN Abhiyaan in 2018 to make India free of malnutrition by 2022. This scheme focuses on improving nutrition for pregnant women, new mothers, teenage girls, and young children. But, big differences in nutrition levels still remain.
Today’s editorial discusses malnutrition among women and girls in India, despite government efforts like the POSHAN Abhiyaan. This topic is useful for GS Paper I (Women-related Issues) and GS Paper II (Welfare State).
_
Let’s learn!
Why in the News?
The government launched the POSHAN Abhiyaan to end malnutrition by 2022, but it has not achieved its goals.
How does malnutrition in India remain deeply gendered?
|
Why has POSHAN 2.0 failed to improve women’s nutrition significantly?
- Underutilization of Allocated Funds: Despite a large budget, only about 69% of funds were used by December 2022, limiting the programme’s reach and effectiveness. Eg: ₹24,000 crore allocated in 2022-23, but nearly one-third remained unspent.
- Rising Anaemia Rates Despite Investments: Anaemia prevalence among women increased from 53% to 57%between NFHS-4 and NFHS-5, showing no significant improvement. Eg: NFHS-5 data shows anaemia rates rose even after POSHAN 2.0’s interventions.
- Focus on Awareness Over Actual Nutrition: The programme has raised awareness (Jan Andolan) but awareness alone cannot address the root causes of malnutrition such as poverty and food scarcity.
- Ignoring Social and Economic Barriers: POSHAN 2.0 largely addresses food supply and supplementation but does not sufficiently tackle women’s economic dependence and decision-making power. Eg: 49% of women lack control over how their income is spent, limiting their ability to benefit from nutrition programmes.
How does women’s empowerment impact nutritional outcomes?
- Improved Spending on Nutrition: When women control income, they prioritize food and health for themselves and their families, leading to better nutrition. Eg: Nobel laureate Esther Duflo found that women’s control over extra income increases spending on children’s nutrition.
- Greater Decision-Making Power: Empowered women can make choices about their diet, healthcare, and food allocation, reducing malnutrition risks. Eg: NFHS-5 showed that women with decision-making power over finances had better nutritional status.
- Increased Access to Employment and Income: Economic empowerment through stable jobs helps women afford nutritious food and healthcare. Eg: Women with even modest independent income were found less likely to be undernourished in low-income communities.
- Enhanced Health Awareness and Education: Empowered women tend to have better knowledge of nutrition and health practices, improving family nutrition. Eg: Women participating in financial literacy and health workshops show better child feeding practices.
- Reduced Gender-Based Nutritional Inequality: Empowerment challenges social norms that deprioritize women’s nutrition, leading to more equitable food distribution. Eg: Households where women contribute economically often have less gender disparity in food consumption.
How can inter-scheme convergence tackle gendered malnutrition?
| Note: Inter-scheme convergence is the coordinated collaboration of multiple government programmes across sectors. |
- Integrated Service Delivery: Combining nutrition, health, and livelihood schemes ensures women receive comprehensive support addressing multiple malnutrition causes. Eg: Anganwadi centres providing food supplements along with skill training and job linkages.
- Efficient Resource Utilization: Coordination between departments reduces duplication and optimizes use of funds for women’s nutrition and empowerment. Eg: Joint budgeting for POSHAN Abhiyaan and women’s employment schemes leads to better fund utilization.
- Holistic Empowerment of Women: Linking nutrition programmes with economic and social empowerment schemes increases women’s ability to accessand afford nutritious food. Eg: Combining POSHAN 2.0 with financial literacy and credit schemes for women.
- Targeted Interventions in High-Risk Areas: Collaborative planning allows focused efforts in districts with severe malnutrition, addressing structural and social barriers. Eg: Health, nutrition, and livelihood departments working together in tribal districts to improve women’s nutrition.
- Multi-dimensional Monitoring and Evaluation: Integrated monitoring tracks progress on nutrition and women’s empowerment indicators simultaneously, improving accountability. Eg: Measuring both reduction in anaemia and increase in women’s decision-making power under joint schemes.
What steps can make women active agents in nutrition programmes? (Way forward)
- Enhance Economic Empowerment: Provide women with access to skill training, income opportunities, and financial literacy so they can afford nutritious food and make independent decisions. Eg: Linking Anganwadi centres with local skill development and credit schemes for women.
- Increase Decision-Making Power: Promote women’s participation in household and community decisions related to health, diet, and resource allocation. Eg: Community meetings where women lead discussions on nutrition and health interventions.
- Strengthen Awareness and Capacity Building: Use nutrition programmes to conduct health education, nutritional counselling, and leadership training, empowering women as knowledge bearers and change-makers. Eg: Financial literacy workshops and health awareness sessions at POSHAN Abhiyaan centres.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Highlights of the Sample Registration System (SRS) 2021 Report
Why in the News?
According to the Sample Registration System (SRS) 2021 report, the Total Fertility Rate (TFR) in India remains unchanged at 2.0 children per woman, the same as in 2020.
Also, the annual crude birth rates for Tamil Nadu, Delhi and Kerala are declining at 2x the rate of the national average.
About Sample Registration System (SRS) 2021 Report:
|
Important Highlights of the SRS, 2021:
[A] Birth Rate Trends :

- India’s crude birth rate in 2021 was 3, declining at 1.12% annually between 2016 and 2021.
- Fastest declines were seen in Tamil Nadu (2.35%), Delhi (2.23%), and Kerala (2.05%).
- Other states with above-average decline: Maharashtra (1.57%), Gujarat (1.24%), Odisha (1.34%), Himachal Pradesh (1.29%), Haryana (1.21%), J&K (1.47%).
- Slowest declines: Rajasthan (0.48%), Bihar (0.86%), Chhattisgarh & Jharkhand (0.98%), Assam & MP (1.05%), West Bengal (1.08%), UP (1.09%).
- Rise in registered births noted in 11 regions, including Bihar, Rajasthan, UP, Uttarakhand, West Bengal, J&K, Ladakh, Lakshadweep, Arunachal Pradesh, Mizoram, and Nagaland.
[B] Total Fertility Rate (TFR) and Demographic Shifts:

- India’s TFR in 2021 stayed at 0, unchanged from 2020.
- Highest TFR: Bihar (3.0); Lowest TFR: Delhi and West Bengal (1.4).
- States below or at replacement level:
- TFR 1.5: Tamil Nadu, Andhra Pradesh, J&K, Kerala, Maharashtra, Punjab
- TFR 1.6: Himachal Pradesh, Telangana, Karnataka
- TFR 1.8: Odisha, Uttarakhand
- TFR 2.0: Gujarat, Haryana
- TFR 2.1: Assam
- Age Structure Shift (1971–2021):
- Children (0–14): declined from 41.2% to 24.8%
- Working-age (15–59): rose from 53.4% to 66.2%
- Elderly (60+): increased from 6.0% to 9.0%
- Aged 65+: grew from 5.3% to 5.9%
- Highest elderly population: Kerala (14.4%), Tamil Nadu (12.9%), Himachal Pradesh (12.3%)
- Lowest elderly population: Bihar (6.9%), Assam (7.0%), Delhi (7.1%)
- Mean female marriage age rose from 3 years (1990) to 22.5 years (2021).
| [UPSC 2024] The total fertility rate in an economy is defined as:
(a) the number of children born per 1000 people in the population in a year. (b) the number of children born to a couple in their lifetime in a given population. (c) the birth rate minus death rate. (d) the average number of live births a woman would have by the end of her child-bearing age. * |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Kerala, MH, TN attain SDGs in MMR, U5MR, NMR
Why in the News?
According to the Sample Registration System (SRS) Report 2021, Kerala, Maharashtra, and Tamil Nadu have successfully achieved the UN Sustainable Development Goals (SDGs) related to Maternal Mortality Rate (MMR), Under-Five Mortality Rate (U5MR), and Neonatal Mortality Rate (NMR).
About SDGs (related to MMR, U5MR, NMR):
- Under SDG 3, the goals focus on ensuring healthy lives and promoting well-being for all.
- Target 3.1 aims to reduce MMR to below 70 per 100,000 live births by 2030, with no country exceeding 140.
- Target 3.2 sets the goal to reduce U5MR to 25 or fewer per 1,000 live births and NMR to 12 or fewer per 1,000 live births.
Key Highlights of the Report:
- States meeting MMR target (≤70):
- Kerala (20), Maharashtra (38), Tamil Nadu (49), plus Telangana, Andhra Pradesh, Jharkhand, Gujarat, and Karnataka.
- States/UTs meeting U5MR target (≤25):
- Includes Kerala (8), Tamil Nadu (14), Delhi, Maharashtra, J&K, West Bengal, Karnataka, Punjab, Telangana, Himachal Pradesh, Andhra Pradesh, and Gujarat.
- States/UTs meeting NMR target (≤12):
- Includes Kerala (4), Tamil Nadu (9), Delhi, Maharashtra, J&K, and Himachal Pradesh.
- National improvements:
- MMR dropped from 130 (2014–16) to 93 (2019–21).
- U5MR declined from 45 (2014) to 31 (2021).
- NMR dropped from 26 (2014) to 19 (2021).
- IMR declined from 39 (2014) to 27 (2021).
- Sex Ratio at Birth improved from 899 to 913 (2014–2021).
- Total Fertility Rate reached replacement level of 2.0 in 2021.
- Compared globally (1990–2023), India achieved an 86% reduction in MMR (vs 48% globally), 78% in U5MR (vs 61%), 70% in NMR (vs 54%), and 71% in IMR (vs 58%).
| [UPSC 2023] Consider the following statements in relation to Janani Suraksha Yojna:
1. It is safe motherhood intervention of the State Health Departments. 2. Its objective is to reduce maternal and neonatal mortality among poor pregnant women. 3. It aims to promote institutional delivery among poor pregnant women. 4. Its objective includes providing public health facilities to sick infants up to one year of age. How many of the statements given above are correct? Options: (a) Only one (b) Only two* (c) Only three (d) All four |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Trends in Maternal Mortality (2000-2023), Report
From UPSC perspective, the following things are important :
Prelims level: Maternal Mortality trends, Schemes
Why in the News?
In 2023, India had the second-highest maternal deaths globally, with 19,000 deaths, tied with the Democratic Republic of Congo, and second only to Nigeria. This equated to 52 fatalities daily according to the UN Report.

About the UN Report
- The report, titled ‘Trends in Maternal Mortality 2000-2023’, was prepared by the World Health Organisation (WHO), UNICEF, UN Population Fund, World Bank, and the UN Department of Economic and Social Affairs (population division).
- It provides global data on maternal mortality and highlights the countries with the highest rates of maternal deaths.
Note:
|
Key Highlights of the Report:
- Nigeria had the highest number of maternal deaths with 75,000 deaths, accounting for 28.7% of global deaths in 2023.
- The top four countries (India, Nigeria, DRC, Pakistan) accounted for 47% of global maternal deaths.
- Despite a population similar to India, China had only 1,400 maternal deaths in 2023.
- Maternal mortality globally declined by 40% between 2000 and 2023, due to improved healthcare access.
- COVID-19 caused an additional 40,000 maternal deaths in 2021 due to service disruptions.
- The global MMR remained high, with 260,000 maternal deaths in 2023, one death every two minutes.
India’s Progress in Reducing Maternal Mortality:
- India’s MMR declined by 78% from 362 in 2000 to 80 in 2023 (NFHS 2019-21).
- Institutional deliveries increased from 79% in 2015-16 to 89% in 2019-21, with Kerala achieving 100%.
- Eight states (including Kerala, Maharashtra, Telangana, Tamil Nadu) reduced MMR to below the SDG target of 70 per 100,000 live births.
Various Schemes for Maternal Health in India:
| Scheme | Launched | Objective | Notable Features | Target Beneficiaries |
| Janani Suraksha Yojana (JSY) | 2005 | To reduce maternal and neonatal mortality by promoting institutional deliveries. | Cash incentives, Focus on rural areas, Increased access to institutional deliveries. | Pregnant women from poor socio-economic backgrounds. |
| Pradhan Mantri Matru Vandana Yojana (PMMVY) | 2017 | To provide maternity benefits and promote institutional deliveries. | Cash benefit of ₹5,000 for the first child, Additional incentives for girl child under PMMVY 2.0. | Women pregnant with their first child after 01.01.2017. |
| Janani Shishu Suraksha Karyakaram (JSSK) | 2011 | To eliminate out-of-pocket expenses for pregnant women and sick infants. | Free delivery services, Free transport, Free post-delivery services. | Pregnant women and sick infants in public health institutions. |
| Surakshit Matritva Aashwasan (SUMAN) | 2019 | To provide assured, dignified, and quality healthcare at no cost. | Zero denial policy, Quality of care, Focus on respectful care. | All pregnant women and newborns visiting public health institutions. |
| LaQshya | 2017 | To improve the quality of care in labor rooms and maternity operation theatres. | Focus on improving infrastructure, Monitoring and evaluation, Quality assurance. | Pregnant women receiving care in labor rooms and maternity OT. |
| [UPSC 2023] Consider the following statements in relation to Janani Suraksha Yojna:
1. It is safe motherhood intervention of the State Health Departments. 2. Its objective is to reduce maternal and neonatal mortality among poor pregnant women. 3. It aims to promote institutional delivery among poor pregnant women. Select the correct answer using the code given below: (a) 1 and 2 only (b) 2, 3 and 4 only (c) 1, 3 and 4 only (d) 1, 2, 3 and 4 |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Palna Scheme under Mission Shakti
From UPSC perspective, the following things are important :
Prelims level: Palna Scheme
Why in the News?
The Ministry of Women and Child Development has informed that 1,761 Anganwadi-cum-Creches are operational across the country under the Palna Scheme.
About the Palna Scheme
- Launched to address childcare needs for working mothers, the Palna Scheme provides day-care facilities for children aged 6 months to 6 years.
- In 2022, the National Creche Scheme was reorganized and renamed Palna Scheme under the Samarthya sub-scheme of Mission Shakti.
- It is a Centrally Sponsored Scheme, with a 60:40 funding ratio between the Centre and State/UT Governments (90:10 for North-Eastern and Special Category States). UTs without legislature receive 100% funding.
- Target Audience: Provides services for all mothers (irrespective of their employment status), offering a safe, hygienic, and supportive environment for children.
- Creche Services: Includes day-care, early stimulation, preschool education, nutrition, health check-ups, and immunization support.
Other Creche Schemes:
|
About Mission Shakti
- Mission Shakti is the Ministry of Women and Child Development’s flagship scheme, designed to strengthen women’s safety, security, and empowerment in India.
- The scheme supports women-led development by addressing issues affecting women across their life-cycle.
- Components:
- Sambal: Focuses on women’s safety, with initiatives like the One Stop Centre (OSC), Women Helpline (WHL), and Beti Bachao Beti Padhao (BBBP).
- Samarthya: Empowering women through sub-schemes like Ujjwala, Swadhar Greh, and the Palna Scheme. It integrates support for childcare and maternal health.
- Gap Funding for Economic Empowerment: A new initiative to support financial gaps in women’s enterprises.
| [UPSC 2019] With reference to the Maternity Benefit Amendment Act, 2017, consider the following statements:
1. Pregnant women are entitled for three months pre-delivery and three months post-delivery paid leave 2. This act applies to all organisations with 20 or more employees 3. It has made it mandatory for every organisation with 50 or more employees to have a crèche. Which of the given statements is/are correct? (a) 1 and 2 only (b) 2 only (c) 3 only (d) 1, 2 and 3 |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Tackling the problem of nutrition
From UPSC perspective, the following things are important :
Mains level: Welfare schemes;
Why in the News?
In the upcoming financial year, the government has increased funding for two key schemes—Saksham Anganwadi and Poshan 2.0.
What are the key nutrition-related schemes that received higher allocations in Budget 2025?
|
Why is India’s nutrition challenge not just about food insecurity but also linked to cultural and social factors?
- Dietary Habits Shaped by Culture: Traditional food choices often lack diversity in essential nutrients, leading to malnutrition. According to the National Family Health Survey-5 (NFHS-5), only 11% of breastfed children (6-23 months) receive an adequate diet. Example: Many vegetarian diets in India lack protein, iron, and vitamin B12, increasing anaemia risks.
- Caste and Social Norms Impact Food Access: Historical caste-based discrimination limits access to nutrient-rich foods for marginalized communities. Example: Many lower-caste communities have restricted access to milk and pulses, key protein sources.
- Gender Disparities in Nutrition: Women often eat last and consume less nutritious food compared to men in the family.
- NFHS-5 reports that 57% of Indian women (15-49 years old) are anaemic, significantly higher than men.
- Urbanization and Processed Food Consumption: Rising income levels and urban lifestyles have increased fast food and processed food consumption, leading to diet-related diseases. Around 23% of women and 22.2% of men in India are overweight or obese, according to NFHS-5. Example: High consumption of sugar-laden, fiber-poor packaged foods contributes to rising cases of diabetes and hypertension.
- Limited Nutrition Focus Beyond Maternal and Child Health: National policies prioritize nutrition interventions for pregnant women and children but ignore other vulnerable groups.Elderly populations and working men receive little policy attention, despite being at risk of malnutrition and lifestyle diseases.
- Example: According to NFHS-5, only 27.5% of adults with diabetes were aware of their condition, 21.5% were on treatment, and just 7% had their diabetes under control.
How does the existing nutrition policy overlook certain segments of the population?
- Focus on Women and Children, Ignoring Other Vulnerable Groups: Most policies, like Poshan 2.0 and Saksham Anganwadi, prioritize maternal and child nutrition but neglect other groups. Example: Elderly populations, adolescent boys, and working men rarely receive targeted nutritional support.
- Lack of Attention to Non-Communicable Diseases (NCDs): Policies focus on undernutrition but ignore rising lifestyle-related diseases like diabetes and hypertension. Example: 14% of adults in India require diabetes medication, yet nutrition plans rarely address high sugar and processed food consumption.
- Limited Inclusion of Urban Poor and Middle-Class Nutritional Needs: Urban food insecurity and poor dietary habits are often overlooked in favor of rural nutrition programs. Example: Many urban poor rely on cheap, processed foods with low nutritional value, increasing obesity and micronutrient deficiencies.
- One-Size-Fits-All Approach Ignores Local Dietary Diversity: National policies provide standardized nutrition interventions that may not align with regional food habits. Example: In some tribal areas, traditional nutrient-rich foods like millets are being replaced with government-distributed wheat and rice, reducing diet diversity.
- Inadequate Support for Special Groups (Elderly, Disabled, Recuperating Patients): People recovering from illnesses, trauma, or those with disabilities have special dietary needs that existing policies fail to address. Example: Health and Wellness Centres (HWCs) provide minimal nutrition support for elderly individuals with osteoporosis or post-surgical patients needing high-protein diets.
What steps has taken by the Indian government?
|
Way forward:
- Expand Nutrition Coverage Beyond Maternal and Child Health: Develop inclusive policies targeting adolescents, elderly populations, and working adults. Example: Introduce nutrition programs for non-communicable diseases (NCDs) like diabetes and obesity.
- Promote Region-Specific and Sustainable Diets: Encourage traditional, locally available nutrient-rich foods over a one-size-fits-all approach. Example: Integrate millets and indigenous grains into government nutrition programs.
Mains PYQ:
Q “Poverty and malnutrition create a vicious cycle, adversely affecting human capital formation. What steps can be taken to break the cycle? (2024)
Reason: This question directly addresses the link between poverty and malnutrition and asks for solutions.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[pib] Phase-III of Suposhit Maa Abhiyan
From UPSC perspective, the following things are important :
Prelims level: Suposhit Maa Abhiyan
Why in the News?
Lok Sabha Speaker launched the third phase of the Suposhit Maa Abhiyan, a campaign aimed at empowering mothers and improving the health of pregnant women and newborns.
What is Suposhit Maa Abhiyan?
- The Suposhit Maa Abhiyan is a maternal and child health initiative launched by Lok Sabha Speaker Om Birla in March 2020 in Kota, Rajasthan.
- It aims to eliminate malnutrition among pregnant women and newborns by providing nutritional support, medical care, and health awareness.
- Social workers and volunteers identify underprivileged pregnant women. Registration through community outreach programs and online platforms.
- Key Features:
-
- Nutritional Support: Monthly 17 kg nutrition kits for pregnant women.
- Medical Assistance: Regular health check-ups, blood tests, and medication support.
- Health Cards: Track maternal health, nutrition levels, and medical history.
- Adoption Model: One pregnant woman per family can be adopted for support.
- Awareness Drives: Sessions on maternal care, infant nutrition, and postpartum health.
- Mortality Rate Reduction: Increased normal deliveries, healthier newborns, and improved maternal health.
Phases of the Campaign:
- Phase 1 (March 2020):
-
- 1,000 pregnant women received balanced nutrition kits.
- Medical check-ups, medicines, and delivery support provided.
- Phase 2 (May 2022):
-
- 3,000 women received nutrition kits for 9 months.
- Expanded health monitoring and medical consultation services.
- Phase 3 (February 2025):
-
- 1,800+ pregnant women identified for continuous health monitoring.
- Monthly nutrition kits and health card tracking introduced.
PYQ:[2020] In order to enhance the prospects of social development, sound and adequate health care policies are needed particularly in the fields of geriatric and maternal health care. Discuss. [2017] Which of the following are the objectives of the ‘National Nutrition Mission’?
Select the correct answer using the code given below: (a) 1 and 2 only |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
A leap backward for maternity entitlements
From UPSC perspective, the following things are important :
Mains level: Legal Maternity Benefit;
Why in the News?
All pregnant women in India are entitled to maternity benefits, yet the majority have not received any financial support in recent years.
What are the legal maternity benefit provisions under the National Food Security Act (NFSA) 2013?
- Universal Entitlement (Except Formal Sector): All pregnant and lactating women (excluding those already receiving maternity benefits in the formal sector) are legally entitled to receive ₹6,000 per child to support nutrition and health.
- Objective of Nutrition and Health Support: The provision aims to improve maternal and child health by ensuring better access to nutrition, rest, and medical care during pregnancy and after childbirth.
- Legal Obligation for Central Government: It is the legal duty of the central government to ensure maternity benefits are provided without arbitrary reductions or restrictions.
How do they compare to the benefits provided under the Pradhan Mantri Matru Vandana Yojana (PMMVY)?
|
What are the issues related to Scant information?
- Minimal Data Disclosure: The Ministry of Women and Child Development provides limited information on PMMVY, violating Section 4 of the RTI Act, which mandates proactive disclosure of public data. For example, basic details like the number of beneficiaries and payment status are not available.
- RTI-Driven Insights: Information on PMMVY coverage is only accessible through RTI queries. For instance, RTI data revealed that effective coverage dropped from 36% in 2019-20 to just 9% in 2023-24, highlighting the program’s declining reach.
- Budgetary Secrecy: There is little transparency about financial allocations and expenditures. For example, official records do not openly explain why central government spending fell to ₹870 crore in 2023-24—just one-third of the amount five years earlier.
Why has the effective coverage of the PMMVY declined sharply since 2019-20?
- Software-Related Issues and Technical Glitches: In 2023-24, major changes in the PMMVY’s software and implementation processes caused frequent system failures, delaying or blocking payments. Officials admitted to facing software issues “every day,” leading to a reduced disbursement rate despite consistent applications.
- Restrictive Eligibility and Complex Documentation: PMMVY limits benefits to only the first child (and a second child if a girl), violating the universal entitlement under the NFSA. Strict Aadhaar-based verification and other conditions exclude migrant workers and women in remote areas who struggle to complete the paperwork.
- Budget Cuts and Reduced Government Spending: Central government spending on PMMVY fell to ₹870 crore in 2023-24, just one-third of the amount five years earlier. This underfunding directly reduced the number of eligible women receiving maternity benefits.
How do the maternity benefit schemes in Tamil Nadu and Odisha differ from the PMMVY?
- Higher Financial Assistance: Tamil Nadu provides ₹18,000 per child (with a promise to increase it to ₹24,000), and Odisha offers ₹10,000 per child. In comparison, PMMVY provides only ₹5,000 for the first child (and a second child if a girl), which is below the ₹6,000 mandated by the NFSA.
- Inclusive Eligibility Criteria: Tamil Nadu and Odisha offer benefits for every childbirth without restrictive conditions. PMMVY, however, limits benefits to the first child (with a recent extension to the second child if a girl), excluding many eligible women.
- Better Implementation and Coverage: Tamil Nadu achieved 84% coverage in 2023-24, and Odisha covered 64% of births in 2021-22. In contrast, PMMVY’s effective coverage fell to just 9% in 2023-24 due to software glitches, reduced spending, and complex documentation.
What role did software-related problems play in further reducing disbursements in 2023-24?
- Frequent System Failures: Major changes in PMMVY’s software and implementation processes in 2023-24 caused regular technical glitches, disrupting the payment system and delaying disbursements. Officials reported encountering software issues daily.
- Reduced Disbursement Rate: Despite consistent applications, technical problems led to a sharp decline in the actual release of benefits. The disbursement rate dropped significantly, contributing to a fall in effective coverage to just 9% in 2023-24.
Way forward:
- Simplify Implementation and Strengthen Technology Infrastructure: Ensure robust, user-friendly software systems with regular maintenance to prevent glitches. Simplify application processes and reduce bureaucratic hurdles for timely disbursement.
- Expand Coverage and Increase Funding: Align PMMVY benefits with NFSA provisions by providing ₹6,000 for every child. Increase budgetary allocations to ensure universal access and include marginalized groups like migrant workers.
Mains PYQ:
Q What are the salient features of the National Food Security Act, 2013? How has the Food Security Bill helped in eliminating hunger and malnutrition in India? (UPSC IAS/2021)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[pib] GARBH-Ini-DRISHTI: India’s First Ferret Research Facility
From UPSC perspective, the following things are important :
Prelims level: GARBH-INi-DRISHTI
Why in the News?
India’s first Ferret Research Facility, GARBH-Ini-DRISHTI, was inaugurated at Translational Health Science and Technology Institute (THSTI) in Faridabad to boost vaccine development and infectious disease research.
About GARBH-INi-DRISHTI
- GARBH-INi-DRISHTI is a data repository and information-sharing hub designed to provide comprehensive clinical and biological insights into maternal and child health.
- Developed under the GARBH-INi program, it is one of South Asia’s largest pregnancy cohort datasets, offering access to clinical data, medical images, and bio-specimens.
- The platform includes data from over 12,000 pregnant women, newborns, and postpartum mothers, enabling extensive research into maternal and neonatal health outcomes.
- It is a collaborative initiative, involving India’s top research institutions and hospitals, ensuring scientific synergy in maternal healthcare.
- Aims:
- To enhance maternal and neonatal healthcare research through large-scale data accessibility.
- To support global researchers in conducting transformative studies that can improve birth outcomes.
- To provide early insights into pregnancy-related complications, fostering better diagnostic and preventive measures.
- To develop predictive tools for conditions like preterm birth, ensuring better maternal health interventions.
- Features:
- Comprehensive Data Repository: Houses clinical, imaging, and bio-specimen data from thousands of pregnant women and newborns.
- Advanced Data Access: Researchers can explore detailed datasets to study pregnancy outcomes, foetal health, and postnatal development.
- Secure and Controlled Access: Provides clear guidance on data usage and approvals, ensuring ethical research practices.
- Global Research Platform: Enables nationwide and international collaboration, allowing researchers to work on common healthcare challenges.
- Supports Policy and Decision-Making: The data can be leveraged to shape maternal health policies, improve diagnostic protocols, and design effective interventions.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[30th January 2025] The Hindu Op-ed: Bridge the milk divide for a nutritionally secure India
PYQ Relevance:Q.) How far do you agree with the view that the focus on the lack of availability of food as the main cause of hunger takes the attention away from ineffective human development policies in India? (CS Mains 2018) |
Mentor’s Comment: UPSC Mains has always focused on the main cause of hunger (2018) and poverty and hunger in India (2019).
India’s White Revolution made it the world’s top milk producer, but now the focus should shift to ensuring milk reaches the most vulnerable. Milk is an important source of protein and calcium, especially for children. However, there are significant differences in milk consumption across income groups and regions. Addressing these gaps is crucial for better health outcomes.
Today’s editorial discusses how milk should be accessible to everyone in India and highlights the differences in milk availability. It looks at how these issues are connected to topics in GS Paper 1, 2, and 3, such as social inequalities, health, and policy solutions.
_
Let’s learn!
Why in the News?
The challenge is making sure that the most vulnerable people have fair access to milk, while also controlling how much milk is consumed by wealthier people.
What is the disparity in milk consumption?
- Income-Based Disparities: Households in the top-income decile consume 3-4 times more milk per capita compared to those in the lowest-income decile. Despite increases in milk consumption among lower-income groups, the poorest 30% account for just 18% of India’s milk.
- Urban vs. Rural and Regional Disparities: Urban households consume ~30% more milk per capita than rural households, despite rural areas being the main milk producers.
- Additionally, northern states like Rajasthan, Punjab, and Haryana have higher consumption (333g-421g), while eastern states like Chhattisgarh, Odisha, and West Bengal have much lower consumption (75g-171g).
- Social Group Disparities: Scheduled Tribe households consume 4 litres less milk per capita annually compared to general category households, highlighting social and economic inequalities in milk access.

What are the nutritional implications of milk consumption in India?
- Protein Source: Milk is a rich source of high-quality protein. In India, it contributes significantly to daily protein intake, especially for children and adults in rural areas. According to the National Family Health Survey (NFHS), over 70% of children in India consume milk, making it a key protein source.
- Calcium and Bone Health: Milk provides essential calcium, which is vital for bone health. Around 67% of Indian households consume milk, helping to prevent calcium deficiency, particularly in growing children and elderly populations, which can lead to conditions like osteoporosis.
- Micronutrients and Vitamin D: Milk is also a good source of vitamins such as B12 and D, essential for immune function and energy production. The National Institute of Nutrition (NIN) states that milk helps in reducing vitamin D deficiency, which is prevalent in India due to limited sunlight exposure.
How can policy interventions address disparities in milk production and access?
- Enhancing Milk Provision: Increase milk availability for vulnerable populations through government schemes like the Pradhan Mantri Poshan Shakti Nirman (POSHAN) and Integrated Child Development Services. States can collaborate with nutrition institutes to align milk products with local dietary preferences.
- Financial Support: Boost financial allocations for existing schemes to ensure adequate milk provision, especially in states where such programs have been discontinued due to budget constraints.
- Nutritional Awareness Campaigns: Conduct awareness campaigns focusing on the benefits of milk consumption, targeting women through various community channels. This can help improve dietary diversity within households.
What strategies can be implemented to promote sustainable dairy practices?
- Healthy Consumption Awareness: Develop partnerships with healthcare professionals and media to promote balanced diets and moderation in dairy consumption among affluent groups.
- For example, Campaigns similar to the UK’s Change4Life initiative could serve as effective models for India.
- Investing in Dairy Infrastructure: The government should continue investing in dairy infrastructure, including animal health care and fodder availability, to ensure sustainable production practices while improving yields.
- Community Engagement: Engage local communities in sustainable practices through education and training programs aimed at improving animal husbandry practices and enhancing productivity without compromising environmental sustainability.
What are the steps taken by the government?
|
Way forward:
- Increase Access for Vulnerable Groups: Expand milk distribution through government schemes (e.g., POSHAN and ICDS) and ensure adequate funding to cover vulnerable populations.
- Regional and Social Equity: Implement targeted interventions to reduce regional, income, and social disparities in milk access, such as milk coupons or subsidies for underserved areas.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Why are fertility levels declining in India?
From UPSC perspective, the following things are important :
Mains level: Issues related to population;
Why in the News?
The Global Burden of Diseases Study (GBD) 2021 shows that India’s fertility rate has dropped significantly, from 6.18 children per woman in the 1950s to 1.9 children per woman in 2021.

What has a GBD Report shown about the total fertility rate in India?
- Declining Fertility Rates: India’s TFR has dramatically decreased from 6.18 in the 1950s to 1.9 in 2021, which is below the replacement level of 2.1 necessary for population stability.
- Future Projections: The report projects that India’s TFR could further decline to 1.04 by 2100, indicating a potential average of less than one child per woman.
- Socio-Economic Concerns: This steep decline in fertility has raised alarms regarding political and socio-economic impacts, particularly in southern states, where there are fears of losing parliamentary representation due to demographic shifts post-delimitation in 2026.
Why are fertility levels declining in India?
- Early Adoption of Family Planning Policies: Southern states like Tamil Nadu and Andhra Pradesh rigorously implemented family planning policies introduced in the 1950s, leading to a significant decline in fertility rates. For example, Andhra Pradesh currently has a Total Fertility Rate (TFR) of 1.5, comparable to Nordic countries like Sweden.
- Higher Female Literacy and Workforce Participation: Increased educational attainment among women has empowered them to delay marriage and childbirth. This is evident in Kerala, where high literacy rates have contributed to the state achieving replacement-level fertility as early as 1988.
- Changing Societal Norms: Cultural shifts have led to late marriages and smaller families. For instance, women in southern states increasingly prioritize careers and financial independence over traditional roles, contributing to lower fertility rates.
- Urbanization and Economic Pressures: Urban lifestyles and rising costs of living discourage larger families. States like Tamil Nadu and Karnataka have seen fertility rates drop to 1.4 and 1.6 respectively due to urbanization and modern aspirations.
Why are the southern States worried?
- Ageing Population: Southern states like Kerala, Tamil Nadu, and Andhra Pradesh have fertility rates that have fallen below the replacement level of 2.1 children per woman. This decline leads to an increasing proportion of elderly individuals in the population, which is projected to rise significantly.
- For instance, Kerala’s population aged 60 and above is expected to increase from 13% in 2011 to 23% by 2036. This demographic shift results in a smaller working-age population, which can strain economic productivity and increase demands for pensions and healthcare services.
- Political Representation: The upcoming delimitation of parliamentary constituencies, based on population figures from the 2031 Census, raises fears that southern states may lose parliamentary seats due to their slower population growth.
- This potential reduction in representation could diminish their political influence at the national level, especially compared to more populous northern states like Uttar Pradesh and Bihar.
- Economic Strain: With a declining workforce contributing less to the economy through taxes and social security, southern states face challenges similar to those observed in countries with ageing populations, such as Japan and China.
- Migration Issues: As birth rates decline, southern states may increasingly rely on internal migration from northern states to fill labour shortages. However, this reliance could create further socio-economic disparities between regions.
Way forward:
- Equitable Resource Distribution: Implement policies ensuring equitable representation and resource allocation in parliamentary seats post-delimitation to address regional disparities without penalizing states with successful population control measures.
- Support for Ageing Populations: Develop robust social security systems, healthcare infrastructure, and incentives for elder care while promoting skill development and migration-friendly policies to mitigate workforce shortages in southern states.
Mains PYQ:
Q Discuss the main objectives of Population Education and point out the measures to achieve them in India in detail. (UPSC IAS/2021)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Mumps Vaccine
From UPSC perspective, the following things are important :
Prelims level: Measles, Mumps, and Rubella (MMR) vaccine
Why in the News?
Tamil Nadu Government has requested the Centre to consider including the Measles, Mumps, and Rubella (MMR) vaccine in the Universal Immunisation Programme (UIP) due to surge in the Mumps cases across the State.
Tamil Nadu’s UIP currently offers 11 vaccines protecting against 12 vaccine-preventable diseases, including:
|
About Mumps Disease
- Mumps is a contagious viral infection caused by the mumps virus, primarily affecting the salivary glands, leading to swelling near the ears (parotitis), fever, headache, and muscle aches.
- It spreads through respiratory droplets or direct contact with saliva.
- While often mild, complications can include orchitis (testicular inflammation), oophoritis (ovarian inflammation), encephalitis, or hearing loss.
- There is no specific treatment, but supportive care like rest, hydration, and pain management helps.
- Vaccination with the MMR vaccine is the best prevention, offering 78–88% protection.
Which free immunised diseases are provided under the Universal Immunization Programme (UIP)?
- The UIP was launched in 1985 and became part of the National Health Mission in 2005 to provide free vaccination against vaccine-preventable diseases for children and pregnant women.
- The programme now covers 12 diseases, including tuberculosis, polio, diphtheria, pertussis, measles, rubella, hepatitis B, pneumonia, rotavirus gastroenteritis, and Japanese encephalitis.
- Key vaccines added over the years include Hepatitis B (2007), Pneumococcal Conjugate Vaccine (2017), Inactivated Polio Vaccine (IPV), and Measles-Rubella Vaccine.
- The entire cost of vaccines is covered by the Government of India, funded through taxes, with an annual budget of ₹7,234 crore (US$870 million) as of 2022.
- The programme covers all residents of India, including foreign residents, ensuring nationwide access to life-saving vaccines.
- 4 new vaccines have been introduced, including the Adult Japanese Encephalitis vaccine and Pneumococcal Conjugate Vaccine, to address emerging health challenges.
Note:Mission Indradhanush is a health initiative launched by the Government of India on 25 December 2014 by Union Health Minister J. P. Nadda. The mission aims to achieve 90% full immunization coverage in India by 2022, targeting vaccination against eight major vaccine-preventable diseases:
The mission targets 201 districts in its first phase, focusing on areas with the highest number of unvaccinated children, particularly in states like Uttar Pradesh, Bihar, Rajasthan, and Madhya Pradesh. The approach follows similar planning and administration as the Pulse Polio Immunisation (PPI) program. |
PYQ:[2016] ‘Mission Indradhanush’ launched by the Government of India pertains to: (a) Immunization of children and pregnant women. (b) Construction of smart cities across the country. (c) India’s own search for the Earth-like planets in outer space. (d) New Educational Policy. |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Indians need to share contraceptive responsibility
From UPSC perspective, the following things are important :
Mains level: Issues related to family Planning;
Why in the News?
According to NFHS-5, 97% of women and 97.5% of men are aware of modern contraceptives, yet the burden primarily falls on women, with female sterilisation being the most prevalent.
What are the current trends in contraceptive decision-making among Indian couples?
- Dominance of Female Sterilization: As of the latest reports, female sterilisation accounts for 37.9% of total sterilizations, while male sterilisation through vasectomies remains critically low at just 0.3%.
- Decline in Male Sterilization: The use of male sterilization has been steadily decreasing over the past three decades.
- Data from the National Family Health Survey (NFHS) show that the percentage of vasectomies has remained stagnant at around 0.3% in both NFHS-4 (2015-16) and NFHS-5 (2019-20), reflecting a broader trend of declining male participation in family planning.
- Government Targets Not Met: The National Health Policy 2017 aimed to increase male sterilization to at least 30%, a target that remains unmet, indicating systemic issues within the family planning framework.
How does societal perception impact men’s involvement in family planning?
- Perception of Burden: Many men view vasectomy as an undue burden, fearing loss of wages and questioning their masculinity. Women often echo this sentiment, believing that men should not be “burdened” by sterilization responsibilities due to their economic roles.
- Lack of Awareness: There is a widespread lack of awareness regarding the benefits and safety of vasectomies, compounded by misconceptions about their effects on libido and masculinity. This misinformation contributes to low acceptance rates among men.
- Cultural Norms: Traditional gender roles reinforce the notion that women should handle family planning, leading to a lack of male engagement in reproductive health discussions.
What strategies can be implemented to promote shared responsibility in contraceptive use? (Way forward)
- Education and Awareness Campaigns: Initiatives should focus on educating both genders about reproductive health and shared responsibilities through school programs and community workshops. Early sensitization can help normalize discussions around male sterilization.
- Conditional Cash Incentives: Increasing financial incentives for men who opt for vasectomies can encourage participation. Evidence from Maharashtra suggests that cash incentives have led to higher rates of vasectomy acceptance among rural men.
- Training Healthcare Providers: Enhancing training for healthcare workers on no-scalpel vasectomies can improve service delivery, particularly in rural areas with limited access to skilled practitioners.
- Public Awareness Campaigns: Drawing lessons from countries like South Korea and Brazil, India can implement mass media campaigns to reshape societal attitudes towards male contraceptive responsibility, emphasising the safety and simplicity of vasectomies compared to female sterilization procedures.
- Policy Implementation with Concrete Steps: The government should ensure that policies are actionable, with clear steps outlined to achieve targets related to male participation in family planning efforts.
Mains PYQ:
Q Discuss the main objectives of Population Education and point out the measures to achieve them in India in detail. (UPSC IAS/2021)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[pib] Postage Stamp released on Sickle Cell Eradication – 2047
From UPSC perspective, the following things are important :
Prelims level: Sickle Cell Anaemia Elimination;
Why in the News?
Madhya Pradesh marked a significant milestone in public health by unveiling a commemorative postage stamp dedicated to the Sickle Cell Eradication – 2047 initiative.
What is the Sickle Cell Disease (SCD)?
|
What are the key facts about the Sickle Cell Eradication – 2047 Initiative?
| Details | |
| Aims and Objectives | • Complete eradication of sickle cell anemia by 2047. • Awareness and screening in tribal communities. • Accessible diagnosis and treatment, with tools like HPLC. • Genetic counseling for prevention. • Technology-driven monitoring via mobile app and National Sickle Cell Portal. |
| Features of the Program | • Newborn screening and prenatal diagnostics at AIIMS Bhopal. • Nationwide expansion to 17 states by 2047. • Advanced testing with HPLC machines. • Community engagement through support groups and education. |
| Implementation | • Collaborations with institutions like AIIMS Bhopal, Sankalp India, and healthcare providers. • Phased rollout starting with high-prevalence regions in Madhya Pradesh. • Government funding for infrastructure and tech development. • Digital technology for data collection and case management. |
PYQ:[2023] Consider the following statements in the context of interventions being undertaken under the Anemia Mukt Bharat Strategy :
How many of the statements given above are correct? (a) Only one |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
What are the costs of population decline?
From UPSC perspective, the following things are important :
Mains level: Issues related to low fertility rate;
Why in the News?
The Chief Ministers of Andhra Pradesh and Tamil Nadu have recently voiced concerns over the low fertility rates in their states.
What is the current demographic situation, especially in the southern States?
- Falling Fertility Rates: Southern states like Tamil Nadu, Andhra Pradesh, Telangana, and Kerala have fertility rates below the replacement level of 2.1.
- For instance, Tamil Nadu and West Bengal recorded fertility rates of 1.4 (2019-21), and Andhra Pradesh, Telangana, and Kerala at 1.5.
- Ageing Population: These states face an advanced demographic transition with an increasingly ageing population. The share of elderly in Kerala is expected to rise to 22.8% by 2036, in Tamil Nadu to 20.8%, and in Andhra Pradesh to 19%.
- End of Demographic Dividend: With a rising old age dependency ratio — Kerala (26.1), Tamil Nadu (20.5), and Andhra Pradesh (18.5) in 2021 — the demographic window for leveraging a young workforce is closing or has already closed in these states.
What is the likely economic impact?
- Rising Healthcare Costs: The elderly demographic is likely to increase healthcare costs. Southern states, comprising one-fifth of India’s population, accounted for 32% of out-of-pocket cardiovascular healthcare expenditure in 2017-18.
- Reduced Economic Growth Potential: A declining working-age population means a lower potential to reap economic benefits from a young labor force. This demographic shift may impact productivity and economic growth.
- Impact on Women’s Labor Force Participation: Pro-natalist policies to increase fertility may lead to a reduction in women’s participation in the labor force, hindering economic growth further.
What are the political implications?
- Federal Representation Changes: With the 2026 delimitation, seats in Parliament are expected to be adjusted based on population. Southern states could lose representation due to slower population growth, with Tamil Nadu potentially losing nine seats, Kerala six, and Andhra Pradesh five, while northern states like Uttar Pradesh, Bihar, and Rajasthan may gain seats.
- Resource Allocation: Slower-growing southern states contribute more tax revenue yet may receive a smaller share of resources from the central pool, as allocation formulas often consider population.
What are the solutions being considered? (Way forward)
- Pro-natalist Incentives: Some southern leaders advocate incentivizing families to have more children. However, international experiences show limited success with pro-natalist incentives.
- Gender Equity and Family Policies: Policies such as paid maternity/paternity leave, accessible childcare, and employment protections can support sustainable fertility rates without economically disadvantaging women.
- Increasing Working Age and Migrant Inclusion: Extending working lifespans and better integrating economic migrants in social security and political representation can help mitigate the impact of an ageing population.
- Balancing Migration Needs: Southern states, which attract many economic migrants, face challenges as these migrants are still counted in their home states, impacting political representation and resource distribution in the host states.
Mains PYQ:
Q Critically examine whether growing population is the cause of poverty OR poverty is the mains cause of population increase in India. (UPSC IAS/2015)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
What is fortified rice? Why did the Centre extend the initiative for its distribution of schemes
From UPSC perspective, the following things are important :
Mains level: Significance of food fortification;
Why in the News?
On October 9, 2024, the Union Cabinet approved extending the free fortified rice supply under welfare programs until December 2028.
Why Rice Fortification is needed?
|
Process of Rice Fortification:
- Fortified Rice Kernels (FRK): The process involves producing fortified rice kernels that are enriched with essential micronutrients such as Iron, Folic Acid, and Vitamin B12.
- Blending with Regular Rice: These fortified kernels are then blended with regular rice at a ratio prescribed by FSSAI (Food Safety and Standards Authority of India).
- Typically, fortified kernels make up 1-2% of the total rice, ensuring consistent delivery of micronutrients without altering the taste or cooking properties of the rice.
How the Fortification Initiative has fared so far?
- The rice fortification scheme was implemented in three phases between 2022 and March 2024, with the target of achieving universal coverage in all government schemes by March 2024 successfully met.
- Fortified rice is now supplied under major welfare programs like the Targeted Public Distribution System (TPDS), Integrated Child Development Service (ICDS), and PM POSHAN in all states and Union Territories.
- The initiative is fully funded by the central government, highlighting its commitment to tackling malnutrition and ensuring inclusive nutritional security across the country.
How can food fortification help reduce malnutrition in India?
- Combats Micronutrient Deficiencies: Fortifying staple foods with essential nutrients like iron and vitamins helps reduce widespread deficiencies that cause anemia and poor health.
- Wide Reach: Through existing public programs (PDS, ICDS), fortified food reaches vulnerable populations, ensuring consistent nutrient intake for large segments of society.
- Cost-Effective: It offers a scalable, affordable solution to malnutrition, improving health outcomes without significant changes in diets or eating habits.
Way forward:
- Strengthen Monitoring and Quality Control: Implement robust monitoring mechanisms to ensure the consistent quality of fortified rice and its proper distribution across welfare programs to maximize nutritional benefits.
- Raise Awareness and Promote Consumption: Conduct awareness campaigns to educate the public on the health benefits of fortified rice, ensuring higher acceptance and consistent consumption to address widespread micronutrient deficiencies.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
India’s Sickle Cell Challenge
From UPSC perspective, the following things are important :
Prelims level: Sickle Cell Anaemia Elimination;
Mains level: Challenges related to the National Sickle Cell Anaemia Elimination Mission;
Why in the News?
The Prime Minister has reaffirmed the government’s dedication to addressing sickle cell disease, a genetic blood disorder that alters the shape of red blood cells.
About the National Sickle Cell Anaemia Elimination Mission:
|
Challenges faced by the Indian Government:
- High Disease Burden: India has the world’s second-largest burden of sickle cell disease, with over a million affected individuals, primarily in tribal areas.
- Low Treatment Coverage: Only 18% of those affected receive consistent treatment, with significant drop-offs in screening, diagnosis, and treatment adherence.
- Stigma and Misinformation: Social stigma around the disease, myths such as “God’s curse” or “black magic,” and mistrust of public health systems, particularly in tribal areas, result in delayed diagnosis and treatment.
- Treatment Adherence Issues: Challenges include inconsistent availability of medicines like hydroxyurea, long travel distances for treatment, and stock shortages at health centers.
- Poor Vaccination Coverage: Vaccination, which reduces infection rates and improves quality of life, remains inadequate in many affected regions.
- Research and Development: The lack of ongoing research into treatments and understanding of the disease in India, and the unaffordability of emerging therapies like gene therapy, hinder long-term progress.
- Financial and Operational Gaps: Health systems in tribal areas require additional funding and operational strengthening to address region-specific health challenges effectively.
What are the WHO recommendations?
- Early Identification: Implement newborn screening programs to identify sickle cell disease at birth.
- Integration into Health Systems: Sickle cell management should be integrated into national health services. This includes establishing specialized centers for comprehensive care and ensuring that primary healthcare providers are trained in managing sickle cell disease.
- Public Education and Awareness: Conduct public education campaigns to raise awareness about sickle cell disease, reduce stigma, and inform communities about genetic risks and prevention strategies.
- Genetic Counseling: Provide genetic counselling to families, especially in communities with high prevalence, to inform them about the risks of having children with sickle cell disease and the importance of carrier screening.
Mains PYQ:
Q Stem cell therapy is gaining popularity in India to treat a wide variety of medical conditions including leukaemia, Thalassemia, damaged cornea and several burns. Describe briefly what stem cell therapy is and what advantages it has over other treatments. (UPSC IAS/2017)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Ovarian Cancer: Understanding the Silent Killer
From UPSC perspective, the following things are important :
Prelims level: Ovarian Cancer
Why in the News?
- In India, Ovarian Cancer ranks among top three cancers affecting women, accounting for 6.6% of all female cancer cases.
-
- In 2022, India alone reported 47,333 new ovarian cancer cases and 32,978 deaths, emphasizing the critical need for awareness, early detection, and effective treatment.
What is Ovarian Cancer?
| Details | |
| About | Referred to as the “silent killer” due to its subtle symptoms like bloating, pelvic pain, loss of appetite, and frequent urination. Late diagnosis is common. |
| Common Symptoms | • Bloating • Pelvic/abdominal pain • Loss of appetite • Frequent urination • Indigestion, back pain, fatigue, and weight loss |
| Cancer Subtypes | • Type I tumours: Less common, early diagnosis, better prognosis • Type II tumours: More common, aggressive, diagnosed at advanced stages |
| Screening | • No effective screening tests available • CA125 blood test used post-diagnosis but not recommended for routine screening due to limited specificity |
| Genetic Risk Factors | • Linked to mutations in BRCA1/BRCA2 genes, increasing risk by up to 50% • Genetic testing aids in personalized risk management |
| Endometriosis | • Associated with a higher risk of certain ovarian cancers, though overall risk remains low |
| Lifestyle Factors | • Mixed evidence regarding talcum powder usage and its potential link to ovarian cancer • Hair products (dyes, straighteners) may increase risk, though further research is required |
| HRT & Genetic Counselling | • Hormone replacement therapy (HRT) is linked to a higher risk of ovarian cancer • Genetic counselling helps at-risk individuals with preventive measures |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
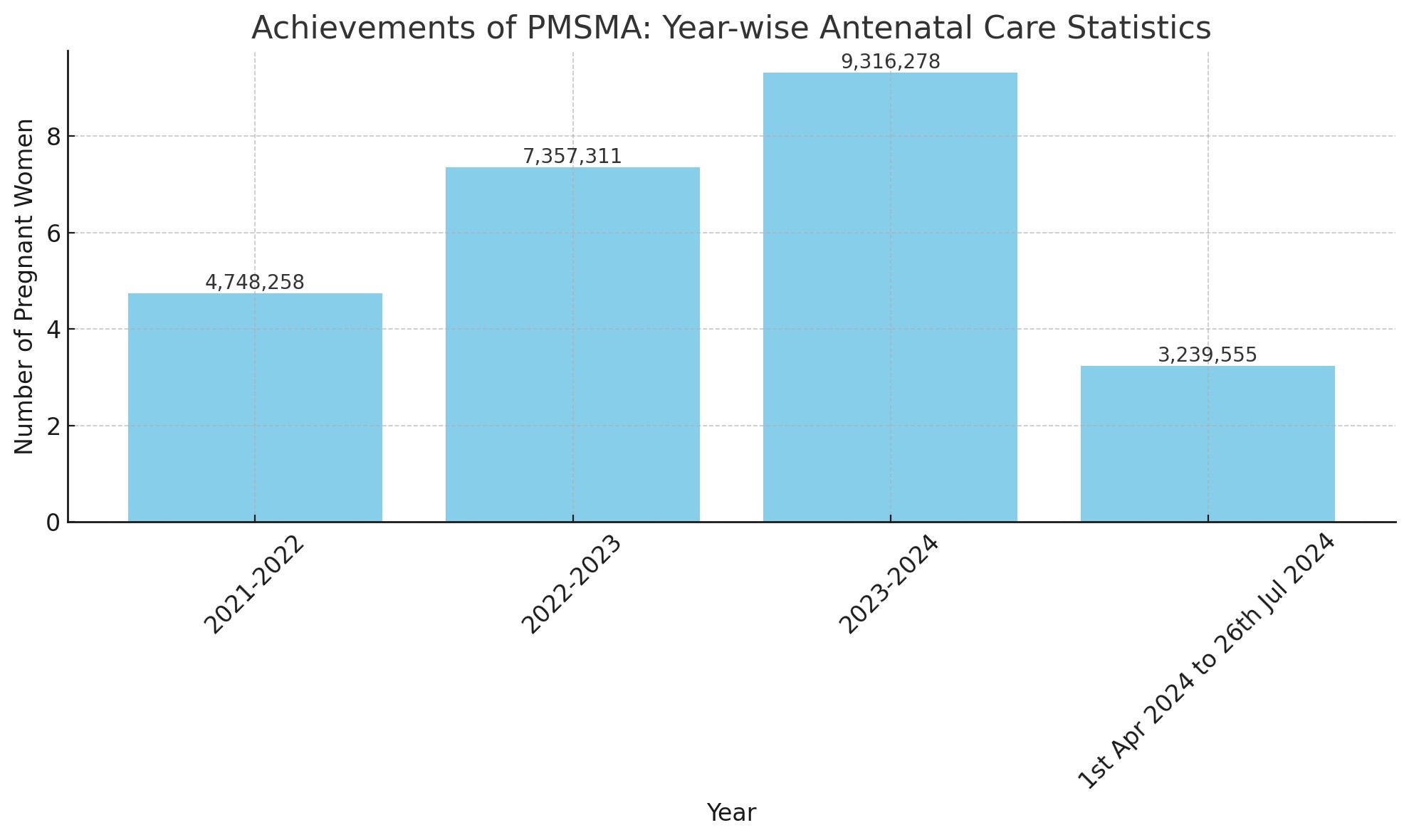
[pib] Update on Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA)
From UPSC perspective, the following things are important :
Prelims level: Features of the Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA)
Why in the News?
- An Extended Pradhan Mantri Surakshit Matritva Abhiyan (E-PMSMA) strategy was launched to ensure quality Antenatal Care (ANC) for pregnant women.
- The strategy focuses on individual tracking of high-risk pregnancies (HRP) and provision of additional PMSMA sessions beyond the 9th of every month.
About High-Risk Pregnancy:
|
About Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA)
| Details | |
| About | An initiative to provide quality antenatal care (ANC) to all pregnant women. |
| Launch | October 2016 |
| Target Group | All pregnant women, especially those in their second and third trimesters. |
| Frequency | Services provided on the 9th of every month at government health facilities. |
| Objective | Ensure safe motherhood by providing comprehensive and quality antenatal care universally. |
| Key Functions |
|
| Key Features |
|
| Categorization of Pregnant Women |
|
| Benefits |
|
PYQ:
[2024] With reference to the ‘Pradhan Mantri Surakshit Matritva Abhiyan’, consider the following statements: 1. This scheme guarantees a minimum package of antenatal care services to women in their second and third trimesters of pregnancy and six months post-delivery health care service in any government health facility. 2. Under this scheme, private sector health care providers of certain specialities can volunteer to provide services at nearby government health facilities. Which of the statements given above is/are correct? (a) 1 only (b) 2 only (c) Both 1 and 2 (d) Neither 1 nor 2 |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[pib] Schemes implemented by the WCD Ministry clubbed into 3 Verticals
From UPSC perspective, the following things are important :
Prelims level: Schemes mentioned in the newscard
Mains level: NA
Why in the News?
- For better implementation and efficient monitoring, all schemes implemented by the Ministry for the betterment of children have been consolidated into 3 verticals:
- These verticals aim to improve nutrition and health indicators, ensure safety and empowerment of women, and provide protection and welfare for children in difficult circumstances.
Scheme Details:
[1] Saksham Anganwadi & Poshan 2.0 (Mission Poshan 2.0)
- The Anganwadi Services Scheme, POSHAN Abhiyaan, and Scheme for Adolescent Girls have been reorganized into three primary sub-verticals:
- Nutrition Support: For POSHAN and Adolescent Girls.
- Early Childhood Care and Education: Targeting children aged 3-6 years.
- Anganwadi Infrastructure: Upgrading and modernizing Saksham Anganwadis.
- Key Features:
- Fortified rice supplied to Anganwadi Centres to meet micronutrient requirements and control anemia among children.
- Emphasis on the use of millets for Hot Cooked Meals at least once a week and Take Home Ration (THR) at Anganwadi centers.
[2] Mission Shakti
- Sambal: Focuses on the safety and security of women.
- Includes schemes like One Stop Centres (OSC), Women Helpline (181-WHL), and Beti Bachao Beti Padhao (BBBP).
- Samarthya: Aims at the empowerment of women.
- Encompasses schemes like Pradhan Mantri Matru Vandana Yojana (PMMVY), Ujjwala, Swadhar Greh (renamed as Shakti Sadan), Working Women Hostel (renamed as Sakhi Niwas), National Hub for Empowerment of Women (NHEW), and National Creche Scheme (renamed as Palna).
[3] Mission Vatsalya
- Objective: To provide better outreach and protection for children in need of care in a mission mode.
- Goals:
- Support and sustain children in difficult circumstances.
- Develop context-based solutions for the holistic development of children from varied backgrounds.
- Encourage innovative solutions through green field projects.
- Facilitate convergent action by gap funding if required.
PYQ:[2016] Which of the following are the objectives of ‘National Nutrition Mission’? 1. To create awareness relating to malnutrition among pregnant women and lactating mothers. 2. To reduce the incidence of anaemia among young children, adolescent girls and women. 3. To promote the consumption of millets, coarse cereals and unpolished rice. 4. To promote the consumption of poultry eggs. Select the correct answer using the code given below: (a) 1 and 2 only (b) 1, 2 and 3 only (c) 1, 2 and 4 only (d) 3 and 4 only |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
How children win with U-WIN, govt’s new online vaccine portal?
From UPSC perspective, the following things are important :
Prelims level: U-WIN
Why in the News?
- The government plans to roll out U-WIN, an online vaccine management portal for childhood vaccination, across the country.
- Similar to CoWIN used during the Covid-19 pandemic, U-WIN aims to digitize and individualize immunization records from birth.
What is U-WIN?
- Children up to 6 years old and pregnant mothers are registered on U-WIN using government IDs like Aadhaar and their mobile phone numbers.
- Records of all 25 shots given to a child and the two given to pregnant mothers are added to the platform.
- It’s Working:
- The platform generates a color-coded vaccination certificate.
- The digital vaccine certificate can be downloaded by parents using their registered mobile numbers, eliminating the need for a physical vaccination booklet.
- After each shot is administered and recorded, the date is added to the card, which also shows the due date for the next set of vaccines.
- U-WIN sends SMS reminders to parents before their children are due for the next dose.
- U-WIN helps locate the nearest vaccination center and book available slots.
Significance:
1) For providing Immunization:
- U-WIN’s reminders to parents are likely to improve compliance with vaccination schedules.
- The platform ensures portability, allowing children to receive their doses anywhere in the country, particularly benefiting children of migrant workers.
- Registration at birth may help reduce the number of “zero dose” children, those who have not received any vaccinations.
2) For Health Workers:
- The platform can automatically generate a due list of children in specific areas for health workers.
- These data points can be utilized by other government programs and eventually connected through the ABHA (Ayushman Bharat Health Account) ID.
Integration with Existing Systems
- U-WIN will link to the government’s existing eVIN platform for inventory management.
- eVIN tracks all vaccine vials, from central stores to each vaccination site, monitoring doses used, wasted, and returned, and tracks real-time temperature and humidity using sensors.
- U-WIN runs on the same principles and digital infrastructure as CoWIN, making adoption straightforward.
- Most vaccinators are familiar with similar platforms, ensuring a smooth transition.
Zero Dose Children
|
PYQ:[2016] ‘Mission Indradhanush’ launched by the Government of India pertains to: (a) Immunization of children and pregnant women (b) Construction of smart cities across the country (c) India’s own search for the Earth-like planets in outer space (d) New Educational Policy |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Do no harm: conservative, non-surgical approaches advised over hysterectomy for gynecological conditions
From UPSC perspective, the following things are important :
Prelims level: Hysterectomy Among Women;
Mains level: Health and disease Issues; Hysterectomy Among Women;
Why in the News?
According to the recent report published in Women’s Reproductive Health under the title ‘Reported Reasons for Undergoing Hysterectomy Among Women Aged 45 Years and Above‘, it was seen that data is lacking on women’s health conditions; thus the true magnitude is never known, impeding funding and escaping the attention of policymakers.
What is Hysterectomy?
Key highlights of the Report:Reasons for Undertaking Hysterectomy:
Frequency of Hysterectomy:
|
Most Cited Reasons for Hysterectomy:
- Primary Reasons:
-
-
- Heavy Menstrual Bleeding or Pain: Cited by 32.1% of women as the reason for undergoing hysterectomy.
- Fibroids or Cysts: Cited by 24.2% of women as the reason for the surgery.
- Uterine Prolapse: Cited by 16.3% of women.
-
- Less Frequently Reported Reasons:
-
-
- Cancer: Among the least reported reasons for undergoing a hysterectomy.
- Severe Post-Partum Hemorrhage is also among the least reported reasons.
-
- Sociodemographic Factors:
-
- Higher risk of undergoing hysterectomy among women from the OBC category, the richest wealth quintile, those with lower education levels, those who married at a younger age, and those with three or more children.
What are the Ministerial guidelines?
- Hysterectomy is a major surgery with a long recovery time and should be considered only after less invasive treatments have been tried.
- The government emphasizes on attempting nonsurgical alternatives in elective cases before opting for a hysterectomy.
Way Forward:
- Healthcare Providers: Train healthcare providers about the potential overuse of hysterectomy and emphasize the importance of considering nonsurgical alternatives.
- Public Awareness: Launch awareness campaigns to educate women about gynecological health, the implications of hysterectomy, and available alternatives.
Mains PYQ:
Q Public health system has limitation in providing universal health coverage. Do you think that private sector can help in bridging the gap? What other viable alternatives do you suggest? (UPSC IAS/2015)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
The impact of 50 years of vaccination on children worldwide
From UPSC perspective, the following things are important :
Prelims level: About Measles Vaccination
Mains level: Global Immunisation Efforts and Current Observations
Why in the News?
On the occasion of World Immunisation Week observed from 24th to 30th April, the Indian Academy of Paediatrics has launched a campaign to focus on routine immunization as the ‘Birth Right’ of a Child.
About Measles Vaccination
- This vaccine protects against 3 diseases: Measles, Mumps, and Rubella (MMR).
- Centre for Disease Control and Prevention (CDC) recommends children get two doses of MMR vaccine, starting with the first dose at 12 -15 months of age, and the second dose at 4-6 years of age. Teens and adults should also be up to date on their MMR vaccination.
Indian Government Initiatives:
- World Immunization Week: The Indian Academy of Paediatrics (IAP) launched a campaign during World Immunisation Week (April 24-30) focusing on routine immunization as a fundamental right of every child. IAP urged the government to expedite the introduction of the HPV vaccine and typhoid conjugate vaccine to address significant public health burdens.
- Vaccination made within the country:
- DTP Vaccine: 93% of surviving infants received the third dose of the DTP vaccine.
- Measles Vaccine: 90% of infants received the second dose of the measles vaccine. The measles vaccine has been the most significant in reducing infant mortality, accounting for 60% of lives saved through immunisation since 1974.
- Present issues include inequitable distribution of vaccines, inability to reach 90% coverage, human resource gaps, and financing problems. In 2022, 33 million children missed a measles vaccine dose, with 22 million missing the first dose and 11 million missing the second dose.
Impacts of Immunisation Globally:
- Lives Saved: Immunisation efforts have saved an estimated 154 million lives globally over the past 50 years, equating to six lives every minute of every year.
- Infant Mortality Reduction: 101 million of the lives saved were infants. Vaccination against 14 diseases has reduced infant deaths by 40% globally and by over 50% in Africa.
- Diseases Targeted: Vaccines have contributed to reducing deaths from diseases like Diphtheria, Haemophilus Influenzae Type B, Hepatitis B, Japanese Encephalitis, Measles, Meningitis A, Pertussis, invasive Pneumococcal disease, Polio, Rotavirus, Rubella, Tetanus, Tuberculosis, and Yellow fever.
Conclusion: Immunisation saves lives, reduces infant mortality, and prevents outbreaks by protecting against infectious diseases, ensuring healthier communities, and securing a better future for children worldwide.
Mains PYQ:
Q What is the basic principle behind vaccine development? How do vaccines work? What approaches were adopted by the Indian vaccine manufacturers to produce COVID-19 vaccines? (UPSC IAS/2022)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Nearly 50% of Pregnancies in India are High-Risk
From UPSC perspective, the following things are important :
Prelims level: Not Muc
Mains level: Maternal health woes in India
Introduction
- Presenting findings from a recent comprehensive study conducted by researchers at the ICMR’s National Institute for Research in Reproductive and Child Health (NIRRCH) in Mumbai.
- Utilizing data extracted from the National Family Health Survey-5 (2019-2021), the study offers a nuanced understanding of the prevalence and determinants of high-risk pregnancies among Indian women.
Pregnancy Issues: Key Statistics
- The study encompasses data from nearly 24,000 pregnant women across India.
- Prevalence of high-risk pregnancies stands at a staggering 49.4%.
- Northeastern states, including Meghalaya (67.8%), Manipur (66.7%), and Mizoram (62.5%), alongside Telangana (60.3%), exhibit the highest prevalence rates.
- Meghalaya records the highest frequency of multiple high-risk factors at 33%.
- Regional disparities in risk factors underscore the imperative for tailored interventions to address local challenges effectively.
Methodology used
- Data Analysis Approach: Employing unit-level data sourced from the Demographic Health Surveys (DHS) program, the study meticulously scrutinizes the prevalence of high-risk pregnancies among women aged 15-49.
- Primary Risk Factors: The study identifies short birth spacing, adverse birth outcomes, and caesarean deliveries as primary contributors to the incidence of high-risk pregnancies.
Major Risks Identified
- Maternal Risks: Critical maternal factors such as age, height, body mass index (BMI), and gestational weight gain emerge as pivotal determinants of pregnancy-related risks.
- Lifestyle and Birth Outcome Risks: Lifestyle choices including tobacco use, alcohol consumption, along with previous birth outcomes significantly influence the likelihood of high-risk pregnancies.
- Educational Disparities: Pregnant women with limited formal education are disproportionately affected, exhibiting heightened prevalence rates of multiple high-risk factors compared to their educated counterparts.
- Temporal Patterns: Notably, high-risk factors tend to escalate during the third trimester, emphasizing the critical need for vigilant monitoring and timely interventions.
Major Government Interventions
- Janani Shishu Suraksha Karyakram (JSSK) (2011): Provides free delivery, including Cesarean section, and essential healthcare services to pregnant women in public health institutions.
- Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA) (2016): Ensures quality antenatal care and high-risk pregnancy detection on the 9th of every month.
- LaQshya Initiative (2011): Aims to improve the quality of care in labor rooms and maternity operation theatres, promoting Respectful Maternity Care.
- Pradhan Mantri Matru Vandana Yojana (PMMVY) (2016): The program aims to provide assured, comprehensive and quality antenatal care, free of cost, universally to all pregnant women on the 9th of every month.
- Surakshit Matritva Aashwasan (SUMAN): Aims to provide assured, dignified, and quality healthcare at no cost for every woman and newborn visiting public health facilities.
- Anaemia Mukt Bharat (2018): Launched with a 6x6x6 strategy to reduce anaemia prevalence among children, adolescents, and women in the reproductive age group.
Way Forward
- Tailored Interventions: Develop region-specific interventions targeting areas with high prevalence rates, addressing local challenges effectively.
- Strengthened Antenatal Care: Ensure access to quality antenatal care services, particularly for women at risk, through initiatives like the Pradhan Mantri Surakshit Matritva Abhiyan.
- Capacity Building: Invest in training healthcare professionals to identify and manage high-risk pregnancies effectively, improving maternal and child health outcomes.
- Integration of Initiatives: Foster coordination and integration among existing government initiatives like Janani Shishu Suraksha Karyakram, Pradhan Mantri Matru Vandana Yojana, and Anaemia Mukt Bharat for holistic maternal care.
Conclusion
- The study advocates for a comprehensive approach aimed at mitigating the prevalence of high-risk pregnancies, safeguarding maternal and child health, and promoting equitable access to healthcare across diverse socio-economic strata.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Early nutrition impacts cognitive development
From UPSC perspective, the following things are important :
Prelims level: Mother’s Absolute Affection Programme
Mains level: addressing child stunting in India requires a multifaceted approach

Central Idea:
Early childhood stunting not only impacts a child’s height but also influences cognitive development, potentially leading to lower educational achievements. The article emphasizes the importance of understanding the underlying mechanisms of this impact, particularly in low- and middle-income countries like India. It discusses a recent study in Ethiopia and Peru, highlighting the negative correlation between stunting at age 5 and later cognitive skills, specifically executive functions. The findings underscore the critical role of early childhood nutrition in determining cognitive development and educational outcomes.
Key Highlights:
- Stunting at around age 5 is linked to lower executive functions, including working memory and inhibitory control, in later childhood.
- Traditional cognitive-achievement tests may not fully capture inherent cognitive skills, and stunting’s impact may extend beyond cognitive deficits to include behavioral factors like delayed school enrollment.
- The article highlights the need for a deeper understanding of the mechanisms through which stunting affects educational achievements, especially in the context of low- and middle-income countries.
Key Challenges:
- Existing research often focuses on specific cognitive-achievement test scores, making it challenging to fully understand the complex relationship between early human capital investments, such as nutrition, and cognitive development.
- Achieving a comprehensive assessment of cognitive skills is complicated by the interplay of cognitive abilities, educational access, and other behavioral factors.
- The article stresses the need to move beyond traditional cognitive-achievement tests and focus on a deeper understanding of the mechanisms linking early human capital investments to cognitive development.
Key Terms and Phrases:
- Early childhood stunting
- Cognitive development
- Executive functions
- Behavioral factors
- Household fixed effects
- Poshan Abhiyaan
- Integrated Child Development Services
- Jal Jeevan Mission
- Swachh Bharat Mission
- Mother’s Absolute Affection Programme
- Complementary feeding
- Anganwadi worker
Key Quotes:
- “Stunting at approximately age 5 is negatively related to executive functions measured years later.”
- “Empirical studies have shown that women’s height and educational attainment are strong predictors of child stunting in India.”
- “Improvements in sanitation reduce the incidence of diarrhoea and stunting.”
- “Promoting early breastfeeding, along with continued breastfeeding for two years, is essential for optimal child development.”
Key Statements:
- The study in Ethiopia and Peru establishes a negative correlation between stunting at age 5 and later cognitive skills, emphasizing the long-term impact of early childhood stunting.
- The article stresses the need to move beyond traditional cognitive-achievement tests and focus on a deeper understanding of the mechanisms linking early human capital investments to cognitive development.
Key Examples and References:
- Sánchez et al.’s study in ‘World Development’ linking early under-nutrition to executive functions in Ethiopia and Peru.
- The role of initiatives like Poshan Abhiyaan, Integrated Child Development Services, Jal Jeevan Mission, and Swachh Bharat Mission in addressing stunting in India.
Key Facts and Data:
- The study in Ethiopia and Peru provides evidence of the negative relationship between stunting at age 5 and executive functions.
- Empirical studies highlight the predictive role of women’s height and educational attainment in child stunting in India.
Critical Analysis:
The article effectively highlights the limitations of traditional cognitive-achievement tests in assessing the impact of early human capital investments on cognitive development. It emphasizes the need for a more nuanced understanding of the complex factors contributing to lower educational achievements, particularly in low- and middle-income countries. The study’s focus on executive functions and the link between stunting and cognitive skills adds valuable insights to the existing literature.
Way Forward:
- Expand initiatives like the Mother’s Absolute Affection Programme to provide comprehensive lactation support and create breastfeeding-friendly environments.
- Implement and scale up community-based complementary feeding programs to educate parents about the importance of a diverse diet for children.
- Consider adding an extra Anganwadi worker to each center to enhance preschool instructional time, potentially improving developmental outcomes and creating employment opportunities.
In summary, addressing child stunting in India requires a multifaceted approach, including comprehensive nutrition initiatives, sanitation improvements, and strategic investments in education and childcare services. The article underscores the need for evidence-based policies to enhance early childhood nutrition and cognitive development.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Govt aims to set up 17,000 creches under Palna Scheme
From UPSC perspective, the following things are important :
Prelims level: Palna Scheme
Mains level: Read the attached story
Central Idea
- The Union Women and Child Development Ministry aims to establish 17,000 creches in Anganwadi centres across the country out of which 5,222 have been approved to date under the ‘Palna’ scheme.
What is Palna Scheme?
| Details | |
| Objective | To provide quality childcare facilities through Anganwadi-cum-Crèches, enabling women’s participation in the workforce |
| Integration | Part of the Samarthya sub-component of Mission Shakti, starting from April 2022
National Creche Scheme (NCS) was revised and subsumed as part of the ‘Palna’ scheme under Mission Shakti. |
| Focus | Establishing combined Anganwadi and crèche facilities for comprehensive childcare |
| Target Demographic | Primarily urban areas where family-based childcare support is less available |
| Standard Operating Procedure | SOP released to outline administrative framework, roles, responsibilities, and monitoring mechanisms |
About National Crèche Scheme (NCS)
| Details | |
| Launch | Rajiv Gandhi National Crèche Scheme (RGNCS) launched in 2006;
From 2017, implemented as the National Crèche Scheme (NCS). |
| Legal Provisions | MGNREGA;
Maternity Benefit (Amendment) Act 2017. |
| Objective | To provide daycare facilities for children aged 6 months to 6 years of working mothers |
| Target Group | Children of working mothers, especially from economically weaker sections of society |
| Childcare Services | Daycare, supplementary nutrition, early childhood education, health check-ups |
| Operational Hours | Typically 7 to 8 hours a day, 26 days a month |
| Age Group | Children aged 6 months to 6 years |
| Administration | Ministry of Women and Child Development, Government of India |
| Execution | Through state governments, NGOs, and community-based organizations |
Try this PYQ from CSP 2019:
Which of the following statements is/are correct regarding the Maternity Benefit (Amendment) Act, 2017?
- Pregnant women are entitled for three months pre-delivery and three months post-delivery paid leave.
- Enterprises with creches must allow the mother minimum six creche visits daily.
- Women with more than two children get reduced entitlements.
Select the correct answer using the code given below.
(a) 1 and 2 only
(b) 2 only
(c) 3 only
(d) 1, 2 and 3
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Private: India’s first Pompe Disease patient passes away
From UPSC perspective, the following things are important :
Prelims level: Pompe Disease
Mains level: NA
Central Idea
- In 2010, Prasanna Shirol established the Organisation for Rare Diseases India, the country’s first NGO dedicated to rare diseases.
- His motivation stemmed from his daughter’s experience with Pompe disease, driving him to provide support and information for others facing similar challenges.
What is Pompe Disease?
- Definition and Cause: Pompe disease, or Glycogen Storage Disease Type II, is a rare genetic disorder caused by a deficiency of the enzyme acid alpha-glucosidase (GAA).
- Enzyme’s Role: GAA is essential for converting glycogen into glucose within cells’ lysosomes.
- Prevalence and Diversity: The disease’s prevalence ranges from 1 in 40,000 to 1 in 300,000 births and affects various ethnicities and populations.
- Variability in Symptoms: The age of onset and severity of Pompe disease can vary, leading to a wide spectrum of clinical presentations.
Impact of Pompe Disease on Individuals
- Muscle Weakness: A primary symptom is progressive muscle weakness, affecting skeletal and smooth muscles, and causing mobility and respiratory issues.
- Motor Skill Development: Children with Pompe disease often experience delays in motor milestones like sitting, crawling, and walking.
- Bone Degeneration: Prolonged muscle weakness can lead to joint contractures and skeletal deformities.
- Respiratory Complications: Weakened respiratory muscles can cause shortness of breath, infections, and potentially respiratory failure.
- Cardiac Issues: The disease can affect heart muscles, leading to symptoms like palpitations, fatigue, and chest pain.
- Hypertrophic Cardiomyopathy: Characterized by thickened heart muscle walls, this condition can impair heart functions.
- Daily Life Challenges: Patients may struggle with daily activities and require assistive devices for mobility and respiratory support.
Diagnosing Pompe Disease
- Enzyme Assays: These tests measure GAA activity to identify enzyme deficiency.
- Genetic Testing: Mutations in the GAA gene are identified through genetic analysis.
- Clinical Evaluation: A comprehensive evaluation of symptoms and medical history is conducted.
- Diagnostic Approach: A combination of enzyme tests and genetic analysis is used for an accurate diagnosis, facilitating timely intervention.
Treatment
- No Cure Yet: Currently, there is no cure for Pompe disease.
- Enzyme Replacement Therapy (ERT): This standard treatment involves infusing the missing enzyme to reduce glycogen buildup, helping manage symptoms and improve quality of life.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
In India, reproductive autonomy remains a pipedream
From UPSC perspective, the following things are important :
Prelims level: MRTP Act
Mains level: Abortion laws, Reproductive autonomy vs ethical considerations
Central idea
- A recent Supreme Court case in India has spotlighted reproductive autonomy. It centers on a 27-year-old mother of two, grappling with an unwanted pregnancy due to lactational amenorrhea, igniting a debate on India’s abortion rights, known for their relative liberalism.
Background
- India’s population policy promotes a two-child norm, making it seemingly unremarkable for a woman to seek an abortion to avoid becoming a mother for the third time.
- However, this case is far from straightforward due to the pregnancy being at 26 weeks, exceeding the gestational limit prescribed in the 2021 Medical Termination of Pregnancy (MTP) Act.
- In such cases, medical practitioners’ opinions hold paramount importance.
Reproductive Autonomy vs. Ethical Concerns
- Interchangeable Terminology: The heart of the matter lies in the interchangeable use of terms like foetus, child, and baby, particularly given the advanced stage of pregnancy. This linguistic flexibility can significantly impact the ethical considerations of the case.
- Concerns of Foeticide: As the pregnancy had reached 26 weeks, concerns emerged regarding the termination possibly constituting “foeticide.” The advanced stage of pregnancy blurs the line between a developing foetus and a potentially viable child, leading to ethical dilemmas.
- Justice Nagarathna’s Emphasis: Justice Nagarathna emphasized the paramount importance of prioritizing the petitioner’s decision and upholding her reproductive autonomy. Her stance echoes Justice D Y Chandrachud’s earlier observation regarding the intrinsic right of pregnant women to choose abortion without the need for consent or authorization from a third party.
- Balancing Reproductive Autonomy and Ethics: The case highlights the intricate balance required between recognizing and safeguarding the fundamental rights of pregnant women to make choices about their bodies and reproductive health, while simultaneously addressing the ethical dimensions of such decisions within the framework of societal values and laws.
The legal framework and amendments pertaining to abortion in India
- MTP Act of 1971: The Medical Termination of Pregnancy (MTP) Act of 1971 was the foundational legislation that regulated abortion in India. It permitted abortions up to 20 weeks of gestation under specific conditions, such as the risk to the life or physical or mental health of the pregnant woman.
- Amendment in 2021: In 2021, the MTP Act underwent significant amendments to modernize and liberalize India’s abortion laws. The key changes included:
-
- Extending the permissible gestational limit from 20 to 24 weeks.
- Expanding access to abortion services by allowing a broader range of healthcare providers to perform abortions, including mid-level providers.
- Constitution of Medical Boards: The 2021 amendment introduced provisions for the constitution of Medical Boards. These boards consist of medical experts responsible for assessing cases where pregnancy termination is sought beyond 24 weeks.
- Reducing Dependency on Courts: By allowing Medical Boards to make determinations, the amendment sought to reduce the burden on the judicial system and expedite the decision-making process for cases involving late-term pregnancies.
Way forward
- Citizen with Agency: The petitioner approached the court as an empowered citizen, asserting her right to make choices about her own body.
- Socially Accepted Context: Her pregnancy occurred within societal norms, emphasizing that reproductive autonomy applies broadly.
- Sound Mental Health: Her rational decision challenges stereotypes about individuals seeking abortions.
- Absence of Foetal Anomalies: Her request is driven by personal choice, not medical necessity.
- Reproductive Choice: She firmly expressed her desire not to have another child, highlighting the importance of individual reproductive decisions.
- Seeking State Support: By seeking state support for safe abortion services, she aligns with international commitments on access to reproductive healthcare as a human right.
Conclusion
- This case underscores the battle between reproductive autonomy and ethical considerations surrounding abortion in India. As women navigate the complex journey to assert their reproductive rights, questions arise about whether they can truly claim ownership of their bodies on their own terms.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Abortion Rights in India: Legal Complexities and Ethical Dilemmas
From UPSC perspective, the following things are important :
Prelims level: MRTP Act
Mains level: Abortion vs. Mothers Bodily Rights

Central Idea
- CJI DY Chandrachud said that India’s abortion law was liberal, pro-choice and far ahead of other countries.
- SC is hearing the case of a married woman who wants to medically terminate her 26-week pregnancy.
- This raises critical questions about a woman’s autonomy in deciding to abort and the existing legislative framework.
Woman’s Perspective
- Unplanned Pregnancy: A 27-year-old married woman, already a mother of two, contends that her pregnancy was unplanned.
- Financial Strain: She argues that her family’s income is inadequate to support another child, and she is undergoing treatment for postpartum depression after her second child’s birth.
Court Decisions and AIIMS Report
- Initial Approval: A two-judge Bench initially allowed the termination, reasoning that an unplanned pregnancy due to contraceptive failure is akin to a forced pregnancy, permitting abortion up to 24 weeks.
- AIIMS Concern: AIIMS, Delhi, raised questions about whether foeticide (stopping the foetal heart) could be performed before termination since the foetus is currently viable.
- Three-Judge Bench: The case was transferred to a three-judge Bench, led by Chief Justice of India (CJI) D Y Chandrachud, which called for a fresh medical report to assess the foetus’s health and the woman’s medical condition.
Understanding the Abortion Law
- Medical Termination of Pregnancy Act (MTP Act): The MTP Act allows termination of pregnancy in three stages.
-
- Termination up to 20 weeks with the advice of one doctor.
- Pregnancy at 20-24 weeks requires the opinion of two registered medical practitioners, under specific conditions.
- After 24 weeks, a medical board in approved facilities assesses the termination based on substantial foetal abnormalities.
Court’s History of Allowing Late-Term Abortion
- Several Precedents: The court has previously permitted terminations beyond 26 weeks in various cases, often in cases of rape or consensual relationships.
- Marital Status Factor: The current case distinguishes itself by the woman’s marital status, implying that the conception is consensual and not a forced pregnancy.
Balancing Rights: Woman vs. Unborn Child
- Ongoing Debate: The CJI-led Bench oscillates between prioritizing a woman’s rights over abortion and the need to balance the rights of the unborn child.
- Liberal Approach: India’s law on abortion is considered liberal and pro-choice, with courts often favouring the woman’s autonomy.
Comparisons with International Standards
- Foetal Viability: The concept of “foetal viability” as a benchmark for abortion approval is relatively new in India. It aligns with international standards.
- US Roe v Wade: The landmark 1973 US Supreme Court case, Roe v Wade, allowed abortion until foetal viability. In 1973, viability was at 28 weeks, now lower due to scientific advancements.
- Criticism of Indian Law: Some critics argue that India’s law lacks clarity as the decision to terminate after 20 weeks falls on doctors rather than the women, leading to frequent court interventions.
Autonomy vs. Unborn Child’s Rights
- Legislative Gap: While the Indian legal framework supports a woman’s autonomy in reproductive decisions, gaps persist, especially concerning last-minute interventions.
- Ethical Debate: The Indian law leans toward women’s autonomy, but ethical dilemmas arise regarding the rights of the unborn child.
- Legal Precedents: Cases like Nand Kishore Sharma versus Union of India have debated the constitutionality of the MTP Act concerning the right to life of an unborn child.
Conclusion
- The ongoing Supreme Court case highlights the intricate legal and ethical considerations surrounding abortion in India.
- While the law supports a woman’s right to choose, the challenge lies in finding a delicate balance between individual autonomy and the rights of the unborn child.
- As the court grapples with this complex case, it underscores the need for continued legal discourse and potential legislative amendments to address evolving reproductive rights issues.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Supreme Court’s divided on Abortion: A Complex Legal Dilemma
From UPSC perspective, the following things are important :
Prelims level: MRTP Act
Mains level: Abortion vs. Mothers Bodily Rights
Central Idea
- A Division Bench of two judges of the Supreme Court grappled with divergent views regarding the abortion of a 26-week pregnancy and the government’s stance to protect the “unborn child.”
- The judges, unable to reach a consensus, opted to refer the case to the CJI to convene a three-judge Bench for further deliberation.
Woman’s Plight for Abortion
- A mother of two with her youngest child just a one-year-old infant, she asserted her desire for a medically induced abortion due to her mental health condition and her inability to care for a third child.
- Her lawyer stressed the court should prioritize the mother’s well-being.
- He emphasized the threat to her privacy and dignity and her conscious decision to not proceed with the pregnancy.
Government’s Stance
- Legal Argument: The Additional Solicitor General contended that the woman did not possess an “absolute right of autonomy” to exercise her reproductive rights in a manner that would compromise the rights of the unborn child.
- MTP Act of 2021: Reference was made to the Medical Termination of Pregnancy (Amendment) Act of 2021, which extended the abortion deadline to 24 weeks in “exceptional circumstances,” primarily to save the mother’s life or in the case of fatal foetal deformity.
Legal Debate
- Bodily Autonomy vs. Foetal Rights: The core of the debate centred on whether, once a viable baby exists, the woman’s right to bodily autonomy or integrity should yield to the Act, curbing her fundamental right to choose.
- Court’s Earlier Decision: On October 9, the Bench had initially permitted the medical termination in line with the woman’s wishes, following a report from an All India Institute of Medical Sciences (AIIMS) medical board.
Government’s Reversal
- Government’s Appeal: Subsequently, the Union government filed an application, citing an expert doctor’s opinion received on October 10, which advocated for giving the child a chance to survive.
- State’s Responsibility: The argument was that a categorical medical opinion had emerged, offering hope for the child’s survival, and placing a responsibility on the state.
Judicial Opinions
- Justice Kohli’s Stance: One judge aligned with the government’s position that the woman should not be allowed to terminate the pregnancy.
- Justice Nagarathna’s Dissent: In contrast, the other judge dissented, asserting that the woman’s decision should be respected, considering her socio-economic circumstances, mental health, and the young age of her second child.
Conclusion
- The Supreme Court’s divided opinion on this intricate abortion case underscores the challenging balance between a woman’s right to make decisions about her body and the state’s interest in protecting the unborn.
- As the case proceeds to a three-judge Bench, it raises broader questions about the legal and ethical complexities surrounding reproductive rights and foetal interests in India’s legal landscape.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Radioactive Chapatis: Concern over a 1969 experiment on South Asian women
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: Medical ethics, Informed consent

Central Idea
- A Member of Parliament in the UK demanded a statutory inquiry into medical research conducted on Indian-origin and South Asian women in Coventry.
- Women of Indian origin were fed Chapatis containing a radioactive isotope of iron, Iron-59 to verify if it treats anaemia.
The 1969 Chapati Study
- The study took place in 1969 and involved approximately 21 Indian-origin women from Coventry.
- These women were given chapatis containing a radioactive isotope of iron, Iron-59, as a part of an effort to combat widespread anaemia.
- The UK’s Medical Research Council (MRC) concluded that the study demonstrated the necessity for increased iron intake among Asian women due to the insolubility of iron in flour.
Ethical Considerations
- The release of the documentary “Deadly Experiments” in 1995 drew attention to the administration of radioactive substances in research during the 1950s and 1960s in the UK and the US.
- Women were unaware of the experiment and its purpose; chapatis were delivered without clear information about their content.
- An independent Committee of Inquiry was established in response to public criticism following the documentary’s release.
- Principles violated in the experiment:
- Informed consent
- Participant-centeredness and
- Transparent engagement
Reflections on Past Practices
- Researchers made judgments about benefits and costs without prioritizing participants’ well-being.
- The study’s design aligned with the prevailing “paternalistic nature of science” and societal attitudes of the time.
- The report suggested providing study materials in participants’ languages and addressing challenges with informed consent.
- Determining informed consent many years later remains a significant challenge.
- The MRC no longer possessed the participant list, and public appeals for participants yielded no results.
Understanding Radioactive Isotopes
- Radioactive isotopes are unstable forms of elements that emit radiation during their transformation into stable forms.
- Unstable nuclei contain excess energy, which is released as radiation in the form of waves or particles.
- The long-term health effects of radiation exposure vary depending on the type and amount of radiation.
Current Repercussions
- An MP emphasized the MRC’s unfulfilled recommendation to identify and engage the women participants.
- Identifying participants would have enabled them to share experiences, receive support, and learn from the experiment.
- The MRC reaffirmed its commitment to engagement, transparency, and upholding the highest research standards.
Conclusion
- The study underscores ethical concerns within historical medical research.
- Reflecting on past practices informs present and future medical research endeavours.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Vital link between Soil Micronutrients and Human Health
From UPSC perspective, the following things are important :
Prelims level: Soil Micronutrients
Mains level: Mother nutrition

Central Idea
- A new study has underscored the significant connection between soil micronutrients and human nutritional outcomes, particularly among children and adult women.
- The research, titled “Soil Micronutrients Linked to Human Health in India,” emphasizes that soil deficiency in key nutrients contributes to nutritional deficiencies in vulnerable populations.
What are Soil Micronutrients?
- Micronutrients are essential elements required by plants in smaller quantities compared to macronutrients (nitrogen, phosphorus, and potassium).
- These micronutrients play crucial roles in various physiological and biochemical processes within plants.
Types of Micronutrients
| Role in Plants | Deficiency Symptoms | |
| Iron (Fe) | Chlorophyll synthesis, photosynthesis | Chlorosis (yellowing) of leaves |
| Manganese (Mn) | Photosynthesis, enzyme activation | Interveinal Chlorosis, poor fruit dev. |
| Zinc (Zn) | Enzyme activity, protein synthesis | Stunted growth, small leaves |
| Copper (Cu) | Enzyme activity, chlorophyll formation | Leaf wilting, reduced growth |
| Molybdenum (Mo) | Nitrogen fixation, enzyme activity | Poor growth, yellowing of leaves |
| Boron (B) | Cell wall formation, auxin synthesis | Distorted growth, reduced fruit dev. |
| Chlorine (Cl) | Osmotic balance, photosynthesis | Osmotic imbalance, leaf damage |
| Nickel (Ni) | Enzyme cofactor | Specific deficiency symptoms |
Soil Micronutrients and Health Correlation
- Soil-Zinc Relationship: The study indicates that districts with higher soil zinc content exhibit lower rates of child stunting and underweight, signifying the importance of soil zinc in nutritional outcomes.
- Height and Soil Zinc: Soil zinc availability corresponds to an increase in the height of women, suggesting a relationship between micronutrient-rich soil and human growth.
- Soil Iron and Anemia: The study highlights a strong connection between soil iron availability and anemia among women, as well as haemoglobin levels in both children and women.
Implications for India
- Soil Nutrient Deficiency: The study holds significance for India, where over 35% of soil is deficient in zinc and around 11% is deficient in iron.
- Micronutrient Deficiency: India faces significant micronutrient deficiency issues, with roughly one-third of the global population experiencing these deficiencies. Iron deficiency is a leading cause of anemia in the country.
Addressing Malnutrition and Stunting
- Malnutrition and Stunting: With a child stunting rate of approximately 39%, malnutrition is a leading risk factor for disability-adjusted life years (DALYs) loss, as per the Lancet’s Global Burden of Disease Study.
- Study Insights: The researchers’ study reveals that a one standard deviation increase in satisfactory soil zinc is associated with a reduction in stunting and underweight among children.
Implications for Policy
- Mitigating Anaemia: The study suggests that soil mineral availability could serve as a valuable tool for mitigating the widespread prevalence of anaemia in the population.
- Wealthier Households: The link between soil zinc availability and childhood stunting is particularly notable in wealthier households, potentially due to additional health constraints that poorer households face.
Way forward
- Soil Enrichment and Agricultural Practices: Implement soil enrichment strategies to address micronutrient deficiencies. Promote sustainable farming practices to enhance soil health and nutrient content.
- Nutrient-Fortified Crops: Invest in research for nutrient-fortified crops rich in essential micronutrients. Encourage the cultivation and consumption of these crops to boost dietary intake.
- Nutritional Education: Launch awareness campaigns about balanced nutrition and micronutrient importance. Educate communities on the role of micronutrients in maintaining good health.
- Women’s Health Programs: Establish tailored health programs for women during pregnancy and lactation. Ensure access to supplements like iron to combat anaemia.
Conclusion
- The study’s findings reaffirm the crucial link between soil micronutrients and human health outcomes, particularly in the context of child stunting, underweight, and anaemia.
- With India grappling with both soil nutrient deficiency and widespread micronutrient deficiencies among its population, this research provides insights that could inform targeted policy interventions.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
India achieves record DPT3 vaccination coverage in 2022: WHO
From UPSC perspective, the following things are important :
Prelims level: DPT3
Mains level: Not Much

Central Idea
- The coverage rate for DPT3 vaccines (diphtheria, pertussis, and tetanus) in India reached an all-time high of 93% in 2022, surpassing the pre-pandemic record of 91% in 2019.
- This significant increase from the 85% coverage in 2021 was reported by the World Health Organization (WHO).
What is DPT3?
- DPT3 vaccines refer to a combination vaccine that provides protection against three infectious diseases: diphtheria, pertussis (whooping cough), and tetanus.
- The “DPT” in DPT3 stands for the initials of these three diseases:
- Diphtheria: It is a bacterial infection that primarily affects the respiratory system. It can cause severe throat and nose congestion, difficulty breathing, and in severe cases, it can lead to heart and nerve damage.
- Pertussis (Whooping Cough): It is a highly contagious respiratory infection caused by the bacterium Bordetella pertussis. It is characterized by severe coughing fits, often accompanied by a “whooping” sound when gasping for breath. Pertussis can be particularly dangerous for infants and young children.
- Tetanus: Also known as lockjaw, is a bacterial infection caused by the bacterium Clostridium tetani. It enters the body through wounds or cuts and produces a toxin that affects the nervous system, leading to muscle stiffness and spasms, particularly in the jaw and neck muscles.
WHO records on immunization
- DPT3 Coverage Recovery: The WHO South-East Asia Region saw the DPT3 coverage recover to pre-pandemic levels of 91% in 2022, a significant increase from 82% in 2021.
- Measles Vaccine Coverage: The region also witnessed a six percent improvement in measles vaccine coverage, rising to 92% in 2022 from 86% in 2021.
- Zero-Dose Children: The number of zero-dose children (those who have not received even the first dose of the DPT vaccine) halved from 4.6 million in 2021 to 2.3 million in 2022.
- Partially Vaccinated Children: The number of partially vaccinated children (those who received at least one dose but not the complete three-dose series) decreased from 1.3 million in 2021 to 650,000 in 2022.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Connection between Anaemia and Maternal Health
From UPSC perspective, the following things are important :
Prelims level: Anaemia
Mains level: Anaemia and Maternal Health

Introduction
- Recent discussions in India have brought anaemia to the forefront, with debates surrounding the measurement and management of haemoglobin levels.
- The WOMAN-2 trial collaborators published a study in The Lancet, emphasizing the importance of anaemia in postpartum haemorrhage and calling for informed policy decisions in India.
- Anaemia affects a significant number of women worldwide and is associated with high mortality rates in postpartum haemorrhage cases.
What is Anaemia?
- Anaemia is a medical condition characterized by a decrease in the number of red blood cells or a deficiency in haemoglobin, the protein responsible for carrying oxygen throughout the body.
- This condition can lead to a reduced capacity of the blood to deliver oxygen to tissues and organs.
- The symptoms of anaemia can vary depending on the underlying cause and the severity of the condition.
However, some common symptoms of anaemia include:
- Fatigue and weakness: Feeling tired and having a lack of energy is a common symptom of Anaemia. This occurs because the body’s tissues and organs do not receive enough oxygen.
- Shortness of breath: Due to the reduced oxygen-carrying capacity of the blood, individuals with Anaemia may experience difficulty breathing, especially during physical activity or exertion.
- Rapid or irregular heartbeat: In an attempt to compensate for the lack of oxygen, the heart may beat faster or irregularly. This symptom is particularly noticeable during physical activity or when the individual is at rest.
- Dizziness and light-headedness: Anaemia can cause a decrease in blood flow to the brain, leading to feelings of dizziness and lightheadedness.
- Cold hands and feet: Reduced blood flow can result in a sensation of coldness in the extremities, such as the hands and feet.
- Headaches: Some individuals with anaemia may experience frequent headaches, which can be a result of the decreased oxygen supply to the brain.
How Anaemia is linked to maternal risks?
- Increased risk of complications: Anaemia during pregnancy raises the risk of preterm birth, low birth weight, and maternal mortality.
- Fatigue and weakness: Anaemia can cause exhaustion, making it harder for pregnant women to handle physical demands.
- Preeclampsia: Anaemia is linked to a higher likelihood of developing preeclampsia, a dangerous condition.
- Postpartum haemorrhage: Anaemia increases the risk of excessive bleeding after childbirth.
- Impaired immune function: Anaemia weakens the immune system, making pregnant women more susceptible to infections.
- Iron deficiency Anaemia: Common during pregnancy, it can negatively impact maternal and fetal health.
Link between Anaemia and Postpartum Haemorrhage
- Global anaemia burden: Over half a billion women of reproductive age suffer from anaemia worldwide.
- Postpartum haemorrhage risk: Anaemia increases the risk of postpartum haemorrhage, a leading cause of maternal deaths, particularly in low- and middle-income countries.
- WOMAN-2 trial: The trial examined the association between prebirth haemoglobin levels and postpartum haemorrhage risk in women from Pakistan, Nigeria, Tanzania, and Zambia.
Findings from the WOMAN-2 Trial
- Continuous relationship: Lower haemoglobin levels were directly associated with increased blood loss and clinical postpartum haemorrhage.
- Impact on maternal function: Women with anaemia experience reduced oxygen-carrying capacity, leading to shock after smaller blood loss volumes.
- Severity of anaemia: Severe anaemia was associated with higher odds of death or near-miss events compared to moderate anaemia.
Recommendations and Prevention Strategies
- Preventive treatment: Attention should be given to preventing and treating anaemia in women of reproductive age.
- Existing initiatives: The Indian government provides iron and folic acid supplements to address anaemia, especially among adolescent girls.
- Challenges and mission-mode approach: Rising levels of anaemia in India require an intensified public health approach to combat the issue effectively.
- Cultural and social considerations: Public health programs should consider cultural attitudes and preferences regarding blood draws for accurate haemoglobin measurement.
- Outreach program considerations: A comprehensive understanding of cultural and social realities is crucial to ensure the success of anaemia prevention initiatives.
Conclusion
- The WOMAN-2 trial highlights the significance of anaemia in postpartum haemorrhage, urging policymakers in India to use evidence-based guidelines for anaemia management.
- The Indian public health program should focus on prevention, treatment, and community engagement to combat rising anaemia levels effectively.
- Cultural and social factors must be considered when designing outreach programs, ensuring their relevance and acceptance by the target population.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
In news: Hematopoietic Stem Cell Transplantations (HSCT)
From UPSC perspective, the following things are important :
Prelims level: Umbilical Cord Blood, Hematopoietic Stem Cell Transplantations (HSCT)
Mains level: Read the attached story

Central Idea: A celebrity couple publicly announced that they had chosen to preserve her baby’s cord blood just a few days before her baby girl was born.
What is Hematopoietic Stem Cell Transplantation (HSCT)?
- What is it? : HSCT is a medical procedure used to treat various disorders affecting the blood, immune system, and metabolism.
- Source of Hematopoietic Stem Cells: Hematopoietic stem cells, which have the ability to develop into different blood cell types, can be obtained from sources such as bone marrow, peripheral blood, or umbilical cord blood.
- Autologous, Allogeneic, and Haploidentical Transplantation: HSCT can involve the use of the patient’s own stored cord blood (autologous), stem cells from a compatible donor (allogeneic), or partially matched stem cells from a family member (haploidentical).
- Procedure Steps: HSCT involves the destruction or suppression of the patient’s abnormal or deficient hematopoietic cells, followed by the infusion of healthy stem cells.
- Commonly Treated Conditions: HSCT is commonly used to treat conditions such as leukemia, lymphoma, aplastic anemia, inherited immune system disorders, and metabolic disorders.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Strengthening ICDS and Empowering Anganwadi Workers
From UPSC perspective, the following things are important :
Prelims level: ICDS Program, Components and related schemes and initiatives
Mains level: ICDS Program, Challenges and potential
Central Idea
- India continues to grapple with high rates of stunting, wasting, and anaemia, posing significant public health risks for children and women. In order to combat these challenges, it is crucial for India to bolster its social sector schemes, particularly the Integrated Child Development Services (ICDS).
What is ICDS?
- ICDS is a flagship program implemented by the Government of India to address the nutritional and developmental needs of children under the age of six, pregnant women, and lactating mothers. The program is implemented through Anganwadi centers, which serve as grassroots-level delivery points for these services in rural and urban areas across the country
key elements of ICDS
- Supplementary Nutrition: ICDS provides supplementary nutrition to children under the age of six, pregnant women, and lactating mothers. This includes the provision of hot cooked meals, take-home rations, and nutritional supplements to address malnutrition and promote healthy growth.
- Immunization: The program ensures the timely immunization of children against preventable diseases. It facilitates immunization sessions and helps families understand the importance of vaccination.
- Health Check-ups: Regular health check-ups are conducted for children and women to monitor their growth, detect any health issues, and provide appropriate medical interventions. This includes weight monitoring, growth assessment, and screening for common ailments.
- Referral Services: ICDS facilitates the referral of children and women to appropriate healthcare facilities for specialized care and treatment when needed. It acts as a link between the community and the healthcare system, ensuring timely access to essential services.
- Non-formal Pre-school Education: ICDS centers provide early childhood education to children aged 3-6 years. This includes age-appropriate learning activities, cognitive stimulation, and socialization opportunities to prepare children for formal schooling.
- Nutrition and Health Education: The program emphasizes the importance of nutrition and health through education and awareness campaigns. Anganwadi workers conduct regular sessions to educate families about proper nutrition, hygiene practices, breastfeeding, and maternal and child health.
- Community Mobilization: ICDS encourages community participation and engagement in the program. It seeks to involve families, community leaders, and local organizations in creating awareness, advocating for children’s rights, and supporting the effective implementation of ICDS services.
- Anganwadi Workers: Anganwadi workers, who serve as the frontline functionaries of ICDS, play a critical role in delivering services at the grassroots level. They are responsible for conducting home visits, implementing program activities, counseling families, and maintaining records.
The Impact of ICDS
- Cognitive Achievements: A study published in World Development revealed the positive impact of ICDS on cognitive achievements, particularly among girls and economically disadvantaged families. The program’s interventions, including nutrition, education, and health services, have shown to contribute to improved cognitive development in children.
- Educational Attainment: Another study published in The University of Chicago Press Journals found that children who were exposed to ICDS during the first three years of life completed more grades of schooling compared to those who did not have access to the program. This indicates that early interventions provided by ICDS positively influence educational outcomes.
- School Enrollment: According to a study published in the Natural Library of Medicine, adolescents aged 13-18, who were born in villages with proper ICDS implementation, showed a 7.8% increased likelihood of school enrollment. This suggests that ICDS plays a role in promoting access to education and increasing enrollment rates.
- Reduction in Malnutrition: The children who remained enrolled in ICDS exhibited reduced rates of child stunting and severe malnutrition. By providing supplementary nutrition and monitoring the growth of children, ICDS contributes to improving nutritional outcomes and addressing malnutrition issues
Why there is need to reassess existing strategies?
- Addressing Persistent Issues: The ICDS program still faces challenges in improving the nutritional and health outcomes for children aged 0-6 years. Despite four decades of efforts, there is a pressing need to reevaluate strategies to effectively tackle these persistent issues.
- Empowering Anganwadi Workers: Empowering Anganwadi workers, who are at the forefront of implementing the ICDS program, is crucial. These workers play a vital role in advancing child nutrition, health, and education in their communities. However, they often face challenges due to high workload and limited resources.
- Variation in Implementation: The significant variation in the implementation of ICDS across different regions and the level of skills of Anganwadi workers. This calls for further investments in training programs to ensure standardized and high-quality service delivery.
- Infrastructural Improvements: The ICDS program also faces infrastructural challenges, such as the lack of functional sanitation facilities, access to potable water, and adequate physical infrastructure in many Anganwadi centers. Addressing these infrastructural gaps is crucial for improving service delivery and overall program effectiveness.
Advantages of Additional Workers to the ICDS Program
- Improved Health and Educational Outcomes: Adding an extra Anganwadi worker to each center can lead to better health and educational outcomes for children. A randomized controlled trial conducted in Tamil Nadu demonstrated that increasing staff levels within the ICDS framework resulted in improved math and language test scores among enrolled children. The additional worker effectively doubled the net preschool instructional time, leading to significant positive effects.
- Reduced Rates of Stunting and Severe Malnutrition: The same trial in Tamil Nadu also showed that children who remained enrolled in the program exhibited reduced rates of child stunting and severe malnutrition. The presence of additional workers can contribute to enhanced nutritional support and monitoring, leading to improved child health outcomes.
- Cost-Effectiveness: Implementing the model of adding an additional Anganwadi worker to each center nationwide is relatively cost-effective compared to the potential benefits it offers. The estimated long-term benefits, based on expected improvements in lifetime earnings, would be around 13 to 21 times the expenses.
- Specialization of Roles: With an additional worker, the responsibilities can be divided to allow existing workers to focus more on child health and nutrition. The new Anganwadi worker can be assigned the specific responsibility of concentrating on preschool and early childhood education. This specialization allows for better utilization of resources and expertise, resulting in improved outcomes in both health and education domains.
- Job Opportunities and Women Empowerment: Adding an extra Anganwadi worker to each center creates job opportunities, particularly for women, across the country. This initiative would lead to the creation of 1.3 million new jobs for women, contributing to economic empowerment and gender equality.
Implementation Challenges Within the ICDS Program
- Variation in Implementation: There is significant variation in the implementation of the ICDS program across different regions of India. This variation can be attributed to factors such as resource allocation, infrastructure availability, and capacity of Anganwadi workers. Addressing this variation and ensuring standardized implementation across all regions is crucial for the program’s effectiveness.
- Skill Levels of Anganwadi Workers: There is a variation in the skill levels of Anganwadi workers. To ensure consistent and high-quality service delivery, it is necessary to invest in training programs that enhance the skills and knowledge of these workers.
- Infrastructural Challenges: Many Anganwadi centers face infrastructural challenges, such as a lack of functional sanitation facilities, inadequate access to potable water, and insufficient physical infrastructure. These infrastructural gaps hinder the effective delivery of ICDS services.
- Decentralized Implementation: The ICDS program operates under a decentralized approach, with state governments overseeing the execution, administration, management, and monitoring of the program. While decentralization promotes tailored implementation, it also poses challenges in terms of coordination, resource allocation, and maintaining consistent standards across different states and regions.
Way Ahead
- Empowerment of Anganwadi Workers: Providing comprehensive support and resources to Anganwadi workers is crucial. This includes enhancing their training programs, improving their skills and knowledge related to child nutrition, health, and early childhood education. Regular capacity-building programs should be conducted to keep them updated with the latest research and best practices.
- Increase Staffing Levels: Adding an additional Anganwadi worker to each existing center can alleviate the workload and ensure more focused attention on preschool and early childhood education. This step would enable existing workers to dedicate more time to child health and nutrition, leading to improved outcomes.
- Improve Infrastructure: Investments should be made to improve the infrastructure of Anganwadi centers. This includes providing functional sanitation facilities, access to clean drinking water, and adequate buildings. Upgrading the infrastructure will create a conducive environment for delivering quality services and ensure the safety and well-being of children.
- Strengthen Monitoring and Evaluation: Robust monitoring and evaluation mechanisms should be established to assess the progress, impact, and effectiveness of the ICDS program. Regular data collection, analysis, and feedback loops will help identify gaps and inform evidence-based decision-making for program improvement.
- Collaborative Approach: Collaboration between the central and state governments, along with active involvement of local communities, is essential. Effective coordination and communication channels should be established to ensure seamless implementation and integration of the ICDS program at all levels.
- Sustainable Funding: Adequate and sustained funding should be allocated to the ICDS program. The government should prioritize investments in child nutrition and early childhood development as a long-term strategy for the nation’s well-being. Exploring partnerships with non-governmental organizations and private sector entities can also help mobilize additional resources.
- Community Engagement and Awareness: Creating awareness among communities about the importance of child nutrition, health, and education is crucial. Community mobilization efforts, including campaigns, workshops, and interactive sessions, should be conducted to engage families and community members in the ICDS program. Promoting behavior change and encouraging active participation will contribute to its success.
- Regular Policy Review: Periodic review and assessment of the ICDS program’s policies and strategies are essential to adapt to changing needs and emerging evidence. Regular policy reviews should be conducted to incorporate best practices, address implementation challenges, and align the program with evolving national and international standards
Conclusion
- To unlock the full potential of ICDS and address persistent issues related to child malnutrition, it is crucial to revisit and re-evaluate its strategies and implementation. Empowering Anganwadi workers through additional staffing, improved training, and better infrastructure is a vital first step. By enhancing the ICDS program, India can make significant progress in improving child nutrition, health, and educational outcomes.
Also read:
| Early Childhood Care and Education through Anganwadis |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Why is India rethinking its Anaemia Policy?
From UPSC perspective, the following things are important :
Prelims level: NFHS, Anaemia
Mains level: Read the attached story
Central Idea
- Anaemia questions are excluded from National Family Health Survey (NFHS-6) due to concerns about accuracy, emphasizing the need for precise estimates to address India’s growing anaemia burden.
- NFHS-5 data reveals a significant increase in anaemia prevalence in India, underscoring the urgency of accurate estimates to effectively tackle this public health challenge.
National Family Health Survey (NFHS)
Each successive round of the NFHS has had two specific goals: 1. To provide essential data on health and family welfare needed by the Ministry of Health and Family Welfare and other agencies for policy and programme purposes, and 2. To provide information on important emerging health and family welfare issues. |
Anaemia: A bigger menace
- Anaemia is characterized by low red blood cells or haemoglobin levels, leading to symptoms like fatigue and weakness.
- Iron deficiency is the primary cause, but deficiencies in folate, vitamins B12, and A also contribute.
- Addressing nutritional deficiencies is crucial for prevention and treatment.
Shift to DABS-I for Anaemia Assessment
- The Health Ministry shifted anaemia assessment to Diet and Biomarkers Survey in India (DABS-I) for more accurate prevalence estimates.
- DABS-I is a comprehensive dietary survey collecting individual data to assess food and nutrient adequacy nationwide.
Reasons for Methodology Change
- Concerns of Over-Diagnosis: Using WHO cut-offs may not suit the Indian population due to various factors that influence anaemia.
- Inadequacy of WHO Cut-Offs: Country-specific cut-offs are needed as the WHO’s haemoglobin cut-offs may not reflect the Indian anaemia situation accurately.
- Differences in Blood Sampling Methods: Venous blood sampling is more accurate than the capillary blood sampling used in previous surveys.
Role of DABS-I Dietary Survey
- DABS-I collects detailed dietary intake data to understand nutritional patterns and deficiencies contributing to anaemia.
- It provides information on nutrient composition in foods from different regions, aiding targeted interventions.
Prevalence of Anaemia in India
- High Burden: Anaemia is a significant public health concern in India, with a high prevalence across different population groups.
- Anaemia among Women: Data from national surveys indicate that a considerable percentage of women in India, particularly those in the reproductive age group, are affected by anaemia.
- Anaemia among Children: Anaemia is also prevalent among children in India, with a substantial proportion experiencing this condition at a young age.
Causes and Risk Factors
- Nutritional Deficiencies: Iron deficiency is the primary cause of anaemia in India. Inadequate intake and absorption of iron, along with deficiencies in other key nutrients, contribute to the problem.
- Socioeconomic Factors: Factors such as poverty, limited access to nutritious food, and inadequate healthcare contribute to the high prevalence of anaemia in certain socioeconomically disadvantaged populations.
- Infections and Diseases: Certain infections, such as malaria and helminthiasis, and chronic diseases like kidney disease and cancer, can increase the risk of developing anaemia.
Impact on Health and Well-being
- Physical Symptoms: Anaemia can cause a range of physical symptoms, including fatigue, weakness, shortness of breath, and impaired cognitive function.
- Maternal and Child Health: Anaemia in pregnant women increases the risk of complications during pregnancy and childbirth. It can also lead to low birth weight and developmental issues in infants.
- Impaired Growth and Development: Anaemia among children can hinder their growth, development, and overall well-being. It may affect cognitive function, school performance, and future productivity.
Government Initiatives and interventions
- National Nutrition Programs: The Government of India has implemented various programs, such as the National Iron+ Initiative and the Pradhan Mantri Matru Vandana Yojana, to address anaemia and improve maternal and child health.
- Supplementation and Fortification: Iron and other micronutrient supplementation programs, along with food fortification initiatives, aim to enhance iron intake and combat anaemia.
- Awareness and Education: Public awareness campaigns and educational programs focus on promoting nutrition, especially among vulnerable groups, and raising awareness about the importance of addressing anaemia.
Challenges and Future Directions
- Access to Healthcare and Nutritious Food: Improving access to quality healthcare services, affordable nutritious food, and clean drinking water is crucial in addressing anaemia in India.
- Multisectoral Collaboration: Addressing anaemia requires collaboration across various sectors, including healthcare, nutrition, education, and social welfare, to develop comprehensive strategies and interventions.
- Monitoring and Evaluation: Regular monitoring and evaluation of anaemia prevalence, intervention effectiveness, and progress towards targets are essential to track improvements and identify areas that require further attention.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Highlights of the Joint Malnutrition Estimates (JME)
From UPSC perspective, the following things are important :
Prelims level: JME Report
Mains level: Malnutrition status in India
Central Idea
- According to the Joint Malnutrition Estimates (JME) by UNICEF, WHO, and the World Bank, India has shown a reduction in stunting among children under five.
Such reports (including NFHS) are credible sources of information to substantiate your answers in Mains answer writing ….
What is Stunting and Wasting?
| Stunting | Wasting | |
| Definition | Impaired growth and development due to chronic malnutrition. | Rapid weight loss and muscle wasting in a short period. |
| Measurement | Height-for-age comparison against standardized growth reference. | Weight-for-height comparison against standardized growth reference. |
| Causes | Insufficient intake of essential nutrients, frequent infections, poor maternal health. | Inadequate caloric intake, poor feeding practices, infectious diseases. |
| Effects | Irreversible consequences, reduced cognitive development, increased disease vulnerability. | Increased morbidity and mortality, severe malnutrition. |
| Time Frame | Long-term condition | Short-term condition |
| Overall Nutritional Status | Reflects chronic malnutrition | Represents acute malnutrition |
| Focus | Impacts growth and development | Impacts weight and muscle mass |
Decline in Child Stunting in India
- The prevalence of stunting in India dropped from 41.6% in 2012 to 31.7% in 2022, with 1.6 crore fewer stunted children recorded.
- India’s share of the global burden of stunting declined from 30% to 25% in the past decade.
Concerns over Wasting
- Wasting remains a concern in India, with an overall prevalence of 18.7% in 2022.
- India contributes 49% to the global burden of wasting, reflecting the severity of this malnutrition indicator.
- Two-thirds of wasting cases in India may be attributed to maternal malnutrition, leading to low birth weight for height.
Rise in Obesity
- The prevalence of obesity in India increased marginally from 2.2% in 2012 to 2.8% in 2022.
- India’s obesity classification remains low compared to the global prevalence of 5.6%.
- Obesity contributes to 8.8% of the global burden, with 31.8 lakh obese children in India.
Way Forward
- The JME report highlights the need for accelerated efforts to achieve global nutrition targets.
- India’s progress aligns with the National Family Health Survey (NFHS) data, indicating a reduction in stunting.
- More research is needed to understand the complexities of wasting, particularly its links to maternal malnutrition.
- Continued focus on addressing malnutrition, access to health services, and maternal nutrition is crucial for further improvement.
- Learning more about wasting and its determinants will be essential for tailored interventions in India and Asia.
Get an IAS/IPS ranker as your personal mentor for UPSC 2024
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Trend of unnecessary Hysterectomies
From UPSC perspective, the following things are important :
Prelims level: Hysterectomy
Mains level: Maternal health issues

Central Idea: The Health Ministry in India is concerned about the high incidence of unnecessary hysterectomies, particularly among poor, less-educated women in rural areas.
Why in news?
- The Supreme Court has directed States and Union Territories to implement health guidelines formulated by the Centre to monitor and prevent unnecessary hysterectomies.
What is Hysterectomy?
- Hysterectomy is a surgical procedure to remove the uterus, and sometimes surrounding organs and tissues.
- It can be classified as a partial hysterectomy (removal of the uterus), total hysterectomy (removal of the uterus and cervix), or radical hysterectomy (removal of the uterus, cervix, part of the vagina, and surrounding tissues).
- The procedure can be performed through the vagina or through an incision in the abdomen.
Issues with such surgery
- Overuse and unnecessary procedures: Hysterectomy can be performed without exploring alternative treatments.
- Psychological and emotional impact: The procedure may lead to feelings of loss and changes in body image.
- Surgical risks and complications: Hysterectomy carries risks such as infection and damage to surrounding organs.
- Long-term health effects: Removal of the uterus may have impacts on hormones and bone health.
- Patient autonomy and informed consent: Patients should be fully informed about the procedure and involved in decision-making.
- Access and equity: Disparities in access to healthcare may contribute to overuse, particularly among marginalized communities.
Concerns and Petition
A public interest litigation (PIL) highlighted the occurrence of unnecessary hysterectomies in the states of Bihar, Chhattisgarh, and Rajasthan under government healthcare schemes.
- Marginalized women were targeted: Women from marginalized communities, such as Scheduled Castes, Scheduled Tribes, and Other Backward Communities, were disproportionately affected.
- Misuse and Insurance Fraud: Healthcare institutions were found to be misusing hysterectomies to claim high insurance fees from the government under various health insurance schemes.
Key issue: Violation of Fundamental Rights
- The recent judgement acknowledges that rising hysterectomy rates among young women in India deviate from trends observed in developed countries.
- It recognizes the violation of fundamental rights, stating that unnecessary hysterectomies infringe upon the right to health and the right to life under Article 21 of the Constitution.
Government action and guidelines
- The Health Ministry has closely monitored the issue of hysterectomies and requested States to share data on hysterectomy cases before and after the implementation of guidelines.
- Compulsory audits for all hysterectomies are advised, similar to those conducted for maternal mortality, in both public and private healthcare institutions.
- In 2022, the Health Ministry issued guidelines to prevent unnecessary hysterectomies and urged States to comply with them.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
India’s Maternal Healthcare Crisis: A Call for Urgent Action
From UPSC perspective, the following things are important :
Prelims level: India's MMR, reports and findings
Mains level: India's high maternal mortality, Government efforts, challenges, and way ahead
Central Idea
- A recent United Nations report revealed a startling reality that India, along with nine other nations, accounted for a staggering 60% of global maternal deaths, stillbirths, and newborn deaths. In 2020 alone, India accounted for over 17% of such fatalities, making it the country with the second-highest number of maternal deaths after Nigeria.
What is maternal mortality?
- As per World Health Organization, Maternal death is the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.
Gaps in maternal Healthcare in India
- Maternal mortality rate: A United Nations report highlighted that India was among the top 10 countries responsible for 60% of global maternal deaths, stillbirths, and new-born deaths. In 2020, India accounted for over 17% of such deaths, making it the second-highest contributor after Nigeria.
- Antenatal care (ANC):1% of mothers in India did not attend any ANC visit during their recent pregnancy. Furthermore, only 34.1% of mothers attended one, two, or three visits, falling short of the World Health Organization’s (WHO) recommendation of four visits.
- Postnatal care: 16% of women in India did not receive any postnatal health check-ups, while 22.8% experienced delayed check-ups occurring two days after childbirth. In the poorest 20% of the households, 26.3% women never had a postnatal health check-up, whereas among the richest, only 7.9% did not.
- Lack of skilled health providers: 8% of Indian women did not receive tetanus shots, which are crucial for preventing infections during and after surgery. In about 11% of cases, no skilled health providers were present at the time of delivery, posing risks in detecting and managing complications.
- Decline in MMR: The Sample Registration System (SRS) 2016-2018 estimated India’s MMR at 113 per 100,000 live births. This represents a decline from previous years and indicates progress in reducing maternal deaths.
Facts for prelims
|
Challenges in achieving further reductions in MMR in India
- Regional Disparities: States with limited healthcare infrastructure and resources often report higher MMR compared to more developed regions. Bridging these regional gaps in healthcare access and quality is crucial for ensuring equitable maternal healthcare outcomes.
- Socioeconomic Factors: Socioeconomic factors play a substantial role in maternal health outcomes. Women from marginalized communities, low-income households, and rural areas face higher risks due to limited access to healthcare facilities, education, and economic resources.
- Quality of Healthcare Services: The availability of skilled healthcare providers, adequate infrastructure, and essential medical supplies is lacking in many parts particularly in remote and ares.
- Awareness and Education: Limited awareness among women, families, and communities about the importance of antenatal care, skilled birth attendance, and postnatal care hindering timely and appropriate care-seeking behavior.
- Cultural and Social Factors: Deep-rooted cultural and social factors often influence maternal healthcare-seeking behavior and decision-making. Traditional beliefs, practices, and societal norms directly or indirectly affect women’s access to and utilization of maternal healthcare services.
Government’s initiatives to improve maternal health
- National Health Mission (NHM): The NHM is a flagship program of the Government of India aimed at providing accessible and affordable healthcare services, including maternal healthcare. Under the NHM, the Reproductive, Maternal, Newborn, Child, and Adolescent Health (RMNCH+A) strategy focuses on improving maternal and child health outcomes through a continuum of care approach.
- Janani Suraksha Yojana (JSY): The JSY is a conditional cash transfer program that encourages institutional deliveries and postnatal care utilization. It provides financial assistance to pregnant women from low-income households to cover the cost of delivery and associated expenses. The program aims to reduce financial barriers and promote institutional deliveries, ensuring access to skilled birth attendants.
- Pradhan Mantri Matru Vandana Yojana (PMMVY): The PMMVY is a maternity benefit scheme that provides cash incentives to pregnant and lactating women for their first live birth. It aims to provide partial wage compensation to pregnant women for wage loss during childbirth and to improve maternal and newborn health outcomes.
- Janani Shishu Suraksha Karyakram (JSSK): The JSSK program ensures free and cashless delivery, including caesarean section, in public health facilities. It covers the costs of essential drugs, diagnostics, blood transfusion, and transportation for pregnant women and sick infants. The program also provides free referral transport services for pregnant women in need of emergency care.
- Maternal Death Surveillance and Response (MDSR): The MDSR system is an important component of the government’s efforts to reduce maternal deaths. It focuses on identifying, reporting, and analyzing maternal deaths to understand the causes and take appropriate actions for prevention in the future.
- National Iron Plus Initiative (NIPI): The NIPI focuses on addressing anemia in pregnant women by providing iron and folic acid supplements. Anemia is a significant risk factor for maternal mortality, and the NIPI aims to ensure universal coverage and adherence to iron and folic acid supplementation during pregnancy.
- Skill Development Initiatives: The government has also emphasized the training and skill development of healthcare professionals, especially in the field of obstetric and neonatal care. This includes the establishment of skilled birth attendant programs, enhancing the capabilities of healthcare providers, and promoting evidence-based practices for safe deliveries and postnatal care.
Way ahead
- Strengthening Healthcare Infrastructure: Investing in healthcare infrastructure, especially in underserved areas, is crucial to improve access to quality maternal healthcare services. This includes ensuring the availability of skilled healthcare professionals, adequate facilities, and essential medical supplies in both urban and rural settings.
- Enhancing Healthcare Workforce: Strengthening the healthcare workforce through training programs and capacity-building initiatives is essential. This involves increasing the number of skilled birth attendants, midwives, and other healthcare professionals who can provide comprehensive maternal care services.
- Improving Access and Affordability: Addressing financial barriers is crucial to ensure that all women can access and afford maternal healthcare services. Enhancing the coverage and effectiveness of health insurance schemes, such as the Pradhan Mantri Jan Arogya Yojana (PMJAY), can significantly reduce out-of-pocket expenses for maternal healthcare.
- Community Engagement and Awareness: Promoting community participation and awareness about maternal health is vital. Community-based programs can play a significant role in educating women, families, and community members about the importance of antenatal care, skilled birth attendance, postnatal care, and recognizing pregnancy-related complications.
- Strengthening Maternal Death Surveillance and Response (MDSR): Enhancing the MDSR system can provide critical insights into the causes of maternal deaths and inform evidence-based interventions. Establishing robust systems for reporting, reviewing, and analyzing maternal deaths can help identify gaps in the healthcare system and facilitate targeted interventions to prevent future deaths.
- Empowering Women and Gender Equality: Promoting gender equality and empowering women are fundamental to improving maternal health outcomes. This includes increasing access to education, economic opportunities, and decision-making power for women. Empowered women are more likely to seek and demand quality maternal healthcare services.
- Collaboration and Partnerships: Collaboration between government agencies, healthcare providers, NGOs, civil society organizations, and other stakeholders is crucial. Partnerships can facilitate the sharing of resources, knowledge, and best practices to drive collective efforts toward reducing maternal mortality rates.
- Monitoring and Evaluation: Establishing robust monitoring and evaluation mechanisms to track progress and identify areas that require further attention is essential. Regular data collection, analysis, and reporting on maternal health indicators can help assess the effectiveness of interventions and inform evidence-based decision-making.
Conclusion
- India’s high maternal mortality rates necessitate immediate interventions to address the gaps in ANC, PNC, awareness, and access to skilled healthcare providers. Bridging the disparities based on education, wealth, and caste is crucial for equitable maternal healthcare. It is imperative to prioritize comprehensive maternal healthcare and take urgent action to save lives and ensure the well-being of women and newborns in India.
Also Read:
| AI to improve maternal and child health in India |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
A Troubling Statistic in India’s Nutritional Landscape
From UPSC perspective, the following things are important :
Prelims level: Statistics on hunger and malnutrition, and initiatives
Mains level: Tackling the problem of hunger and malnutrition
Central Idea
- A troubling statistic in the fifth National Family Health Survey (NFHS-5) data, conducted in 2019-21, is not well-known. Going without food for an entire day at this critical period of a child’s development raises serious concerns related to severe food insecurity.
Statistics from the NFHS-5 data
- Zero-food: Among mothers with a child between ages 6-23 months, 18% reported that their child did not eat any food whatsoever (“zero-food”) in the 24 hours preceding the survey. The zero-food prevalence was 30% for infants aged 6-11 months, 13% among 12-17 months old, and 8% among 18-23 months old.
- Zero-protein: More than 80% of children in the age group of 6-23 months had not consumed any protein-rich foods for an entire day (“zero-protein”). Close to 40% of children in the age group of 6-23 months did not eat any grains (roti, rice, etc.) for an entire day.
- Zero-milk: Six out of 10 children in the age group of 6-23 months do not consume milk or dairy of any form every day (“zero-milk”).
The current measures for undernutrition
- Stunting: It is a measure of chronic malnutrition, where children are too short for their age. It is determined by comparing a child’s height with the World Health Organization (WHO) child growth standards.
- Wasting: It is a measure of acute malnutrition, where children have a low weight for their height. It is determined by comparing a child’s weight with the WHO child growth standards.
- Underweight: It is a measure of both chronic and acute malnutrition, where children have a low weight for their age. It is determined by comparing a child’s weight with the WHO child growth standards.
Limitations of current measures of undernutrition
- Anthropometric measures: The assessment of the extent of nutritional deprivation among young children in India has relied on measures of anthropometric failure such as the percentage of children short for their age (stunting) or weighing less given their height (wasting), compared to a reference population. These measures are, at best, proxies suggesting plausible overall deficiencies in the child’s environment, without any guidance on the specific nature of the deficiencies. They do not provide insight into the specific food groups that are lacking in the child’s diet.
- Multifactorial nature: Given the multifactorial nature of what causes stunting or wasting among children, it is challenging for any single ministry or department of the Government of India to take responsibility for designing, implementing and monitoring policies to reduce undernutrition among children.
- Sensitivity: The sensitivity of the stunting prevalence to what population reference is being used makes it problematic as a policy metric for creating and evaluating the effectiveness of current programs and interventions.
- Lack of data: The fact that we do not know what India eats highlights a core deficiency in data related to food and dietary consumption. This limits the ability to design effective policies and programs to improve nutritional security among Indians.
Facts for prelims
|
Initiative |
Description |
| NFHS-5 | Conducted in 2019-21, it revealed that 18% of mothers with a child between ages 6-23 months reported zero-food intake. |
| Mission Poshan 2.0 | A flagship programme aimed at achieving SDG 2 “zero hunger” and focuses on food-based initiatives. |
| Swachh Bharat Mission (SBM) | Increased access to improved toilets among Indian households from 48% to 70% between 2016 and 2021. |
| Zero Food Metric | A food-based metric that provides a good start to monitor and assess the performance of Poshan 2.0. |
| White House initiative on hunger, nutrition and health | Launched by the US to end hunger by 2030. |
Calorie intake recommendations by WHO
- According to the World Health Organisation, at six months of age, 33 per cent of the daily calorie intake is expected to come from food. This proportion increases to 61 per cent at 12 months of age.
- The recommended calorie percentages mentioned here are the minimum amount that should come from food.
- It is presumed that the child obtains the remaining calories through on-demand breastfeeding, meaning the child is breastfed whenever they need it throughout the day and night, and not solely when the mother is able to provide it.
- Consequently, the percentage of food-sourced calories only increases further when a child cannot receive breast milk when needed.
What is the need for Poshan 2.0?
- Achieving SDG 2: Poshan 2.0 is a flagship program that aims to achieve SDG 2, which aims to end hunger and ensure year-round access to safe, nutritious, and sufficient food by 2030.
- Targeting maternal and child nutrition: Poshan 2.0 focuses on food-based initiatives, including its flagship supplementary nutrition program service as mandated by the 2013 National Food Security Act, to target maternal and child nutrition.
- Developing food-based metrics: To effectively monitor and assess the performance of Poshan 2.0, there is an immediate need to develop appropriate food-based metrics to measure the extent of food insecurity among Indian households.
- Improving nutritional security: The goal of Poshan 2.0 is to ensure affordable access to sufficient quantity and quality of nutritionally diverse food, with a special and immediate focus on India’s youngest children to improve nutritional security among Indians.
- Establishing routine dietary and nutritional assessments: A national effort to establish routine dietary and nutritional assessments for the entire population is the need of the hour to measure the availability, accessibility, and affordability of nutritious food, especially for disadvantaged and vulnerable populations such as young children, and constitute the foundation for any evidence-based policy to end hunger and improve nutritional security among Indians.
Way ahead
- Elevating food intake among young children to be of primary importance, as opposed to being referred to as “complementary” in policies and guidelines related to maternal, infant and young child nutrition.
- Extending the 24-hour recall questions on consumption of various food items to the population of children under five years to better understand food security for all populations in India.
- Developing appropriate food-based metrics to effectively monitor and assess the performance of Mission Poshan 2.0.
- Establishing routine dietary and nutritional assessments for the entire population to measure the availability, accessibility and affordability of nutritious food, especially for disadvantaged and vulnerable populations such as young children.
- Consider a strategic initiative led by the Prime Minister’s Office aimed at eliminating food insecurity in India and ensuring affordable access to sufficient quantity and quality of nutritionally diverse food, with a special and immediate focus on India’s youngest children.
Conclusion
- Given the urgency of the situation and the critical need for prompt action to address the issue of hunger and malnutrition among Indians, it is recommended that India takes inspiration from the United States. Recently, the US launched a high-level initiative aimed at ending hunger by 2030, which could offer valuable insights and guidance to India’s efforts in this direction.
Mains Question
Q. Statistic in the fifth National Family Health Survey (NFHS-5) data on hunger and malnutrition is troubling. In this backdrop discuss the need for Poshan 2.0 for India.
Also Read:
| A reality check on Nutrition programs |
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
What is Garbh-Ini Program?
From UPSC perspective, the following things are important :
Prelims level: Garbh-INI Program
Mains level: NA
Central idea: The scientists working in the Garbh-Ini program have identified 19 single nucleotide polymorphisms (SNPs) or genetic markers that are associated with preterm or premature birth.
What is Garbh-Ini?
- It is an interdisciplinary research program in India that focuses on the advanced research of birth outcomes.
- It is a collaborative initiative under the Department of Biotechnology.
- It is led by DBT-Translational Health Science and Technology Institute (THSTI) in the NCR Biotech cluster, Faridabad, in collaboration with DBT-NIBMG, Kalyani, DBT-Regional Centre for Biotechnology (RCB), Gurugram Civil Hospital, and other organizations.
- The program aims to use advanced technology to improve maternal and child health outcomes and address the high incidence of preterm births in India.
What are Single Nucleotide Polymorphisms (SNPs)?
- Genetic markers are specific sequences of DNA that can be used to identify an individual or a particular trait.
- Single nucleotide polymorphisms (SNPs) are the most common type of genetic variation that occurs in the DNA sequence.
- SNPs occur when a single nucleotide (A, C, T, or G) in the DNA sequence is altered.
- These changes can occur in any region of the genome and can be used as genetic markers to identify specific traits or disease susceptibility.
Significance of the Study
- The study is significant as it identifies 19 SNPs or genetic markers that are associated with preterm or premature birth.
- Out of these 19 SNPs, five were found to be associated with an increased risk of early preterm birth (birth before 33 weeks) and can be used to predict premature births.
- This is the first study in South Asia to identify genetic markers associated with preterm births, and it has significant implications for improving maternal and child health outcomes in India.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Type 1 and Type 2 Diabetes among Children
From UPSC perspective, the following things are important :
Prelims level: Diabates among children
Mains level: Not Much

The National Commission for Protection of Child Rights (NCPCR) has written to Education Boards of all States/UTs, stating schools must ensure proper care/facilities for children with Type 1 diabetes (T1D).
What is Diabetes?
- Diabetes is a chronic medical condition that occurs when the body cannot regulate blood sugar levels properly.
- Blood sugar, also known as blood glucose, is the main source of energy for the body’s cells.
- Insulin, a hormone produced by the pancreas, helps the body use and store glucose from food.
- In diabetes, the body either does not produce enough insulin or cannot use the insulin it produces effectively, resulting in high blood sugar levels.
- Over time, high blood sugar levels can cause serious health problems, such as damage to the heart, blood vessels, eyes, kidneys, and nerves.
Types of Diabetes
There are two main types of diabetes: Type 1 and Type 2.
- Type 1 diabetes: It is an autoimmune disease in which the immune system attacks and destroys insulin-producing cells in the pancreas, resulting in a lack of insulin. This type of diabetes is typically diagnosed in children and young adults, although it can occur at any age. It requires insulin injections or pump therapy for survival.
- Type 2 diabetes: It is a metabolic disorder in which the body becomes resistant to the effects of insulin or doesn’t produce enough insulin to maintain normal glucose levels. This type of diabetes is often associated with lifestyle factors such as obesity, physical inactivity, and poor diet. It is typically diagnosed in adults, but it is becoming increasingly common in children and adolescents as well. Treatment for Type 2 diabetes may include lifestyle changes, oral medications, or insulin therapy.
Menace of diabetes in India
- According to data from the International Diabetes Federation Atlas 2021, India has the world’s highest number of children and adolescents living with Type I Diabetes Mellitus (TIDM).
- There are over 2.4 lakh TID patients in the Southeast Asia region.
Measures to mitigate TID impact on students
- CBSE circular in 2017 allowed students with T1D in Classes X and XII to carry certain eatables to board exam hall to avoid low sugar episodes.
- They are permitted to carry medicines, snacks, water, a glucometer, and testing strips.
- NCPCR suggests states allow students to use smartphones to monitor sugar levels.
- Tamil Nadu has been providing free insulin to children with T1D since 1988.
Back2Basics: National Commission for Protection of Child Rights (NCPCR)
- NCPCR is a statutory body established in India under the Commissions for Protection of Child Rights Act, 2005.
- Its objective is to protect, promote and defend the rights of children in India.
- It functions as a watchdog to prevent child rights violations, as well as to take action against those responsible for such violations.
- The NCPCR also advocates for the implementation of laws, policies and programs aimed at promoting child welfare and development.
Are you an IAS Worthy Aspirant? Get a reality check with the All India Smash UPSC Scholarship Test
Get upto 100% Scholarship | 900 Registration till now | Only 100 Slots Left
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Bengal is tackling fatal Adenovirus Infection
From UPSC perspective, the following things are important :
Prelims level: Adenovirus
Mains level: NA

Central idea: 19 children below the age of five years have died in State-run institutions due to acute respiratory infection (ARI) caused by Adenovirus.
What is Adenovirus Infection?
- Adenoviruses are common viruses that typically cause mild cold or flu-like illness and are usually spread from an infected person to others by close personal contact
- The virus is transmitted through the air by coughing and sneezing and also by touching an object or surface with adenoviruses on it
- While the virus can affect people of any age group, children with low and compromised immunity are at a higher risk
- Symptoms of the viral infection, other than common cold or flu-like symptoms, include acute bronchitis, pneumonia, pink eye (conjunctivitis), and acute gastroenteritis
Reasons for outbreak in Bengal
- Doctors claim that it is the recombinant strain which is the reason for the spike in infections and deaths.
- Most of the children who have been infected by the virus are less than three years old and were born during the COVID-19 pandemic.
- Children who are in the age group of six months to preschool are most susceptible to viral infection.
Are you an IAS Worthy Aspirant? Get a reality check with the All India Smash UPSC Scholarship Test
Get upto 100% Scholarship | 900 Registration till now | Only 100 Slots Left
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Sickle Cell Anaemia screening meets only 1% of target
From UPSC perspective, the following things are important :
Prelims level: Sicke Cell Anaemia
Mains level: Read the attached story

Central idea: The Health Ministry of India set a target to scan one crore people for sickle cell disease in 2022-23. However, with only two weeks left in the fiscal year, the Ministry has completed only 1% of the target.
What is Sickle Cell Anaemia?

- Sickle Cell Anaemia is a genetic blood disorder that affects the haemoglobin molecule in red blood cells.
- People with sickle cell anaemia have abnormal haemoglobin that causes their red blood cells to become sickle-shaped, rigid and sticky.
- These abnormal cells can clog small blood vessels, leading to excruciating pain, organ damage, and a higher risk of infections.
- Sickle cell anaemia is inherited in an autosomal recessive pattern, which means that a person must inherit two copies of the mutated gene, one from each parent, to develop the disease.
- There is no cure for sickle cell anaemia, but treatments are available to manage its symptoms and complications.
How widespread is it in India?
- Sickle cell anaemia is prevalent in some parts of India, particularly in tribal and rural areas.
- According to the ICMR, sickle cell trait is present in about 20-22% of the tribal population in central India, and the disease is present in about 3-5% of the same population.
- It is estimated that there are about 30 million carriers of the sickle cell trait in India, and around 1.5-2 lakh sickle cell disease patients.
- The disease is most commonly found in the states of Chhattisgarh, Madhya Pradesh, Maharashtra, Odisha, and Gujarat.
Recent discussions
- India aims to eradicate sickle cell anaemia by 2047, Finance Minister announced during her Budget 2023 speech.
- Under the new scheme, 70 million people up to the age of 40 years in affected tribal areas will be screened for the disease.
- The Health Ministry has assigned tentative State-wise screening targets to the States for timely completion of the exercise.
- The Ministry is working to create and maintain a central registry for all screened persons to prevent patients from slipping through the cracks.
Current status of screening
- Only 1,05,954 people have been screened so far, out of which 5959 people, or 5.62% of those screened were found to be carrying sickle cell disease traits.
- Regular and timely screening of the population is important, as in a previous screening exercise of over 1.13 crore people in 2016, up to 9,49,057 (8.75%) tested positive for the sickle cell trait, and up to 47,311 of these ended up with full-blown sickle cell disease.
Way forward
- Increased screening: Achieving the goal of eliminating sickle cell anaemia would involve screening at least seven crore people under the age of 40 years in multiple phases by 2025-26.
- Creating awareness: The Health Ministry is working to create awareness amongst those who carry the sickle cell trait to refrain from marrying another person who also carries the trait.
- Targeted assessment: Pregnant women are a priority group for immediate screening, and in the long-term, screening of targeted population of unmarried adolescents between 10 to 25 years will be undertaken.
Are you an IAS Worthy Aspirant? Get a reality check with the All India Smash UPSC Scholarship Test
Get upto 100% Scholarship | 900 Registration till now | Only 100 Slots Left
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Malnutrition in the North-eastern states of India
From UPSC perspective, the following things are important :
Prelims level: Malnutrition, stunting, wasting etc
Mains level: Malnutrition in India
Context
- Between the National Family Health Survey (N

FHS)-4 (2015–16) and the fifth round (2019–2020), there has been a considerable increase in the number of malnourished children in India, and the progress made during the first half of the decade appears to have been undone. Malnutrition in the North-eastern states of India is worse than the country average.
Crack Prelims 2023! Talk to our Rankers
What is malnutrition?
- Malnutrition refers to deficiencies, excesses or imbalances in a person’s intake of energy and/or nutrients.
- For a child’s motor, sensory, cognitive, social, and emotional development, malnutrition has substantial long-term effects. It impedes productivity and academic progress.
The term malnutrition covers two broad groups of conditions
- Undernutrition: Undernutrition includes stunting (low height for age), wasting (low weight for height), underweight (low weight for age) and micronutrient deficiencies or insufficiencies (a lack of important vitamins and minerals).
- Overnutition: The other is overweight, obesity and diet-related non-communicable diseases (such as heart disease, stroke, diabetes, and cancer).
Did you know?
- Stunting, or low height for age, is a recognized risk factor for children’s delayed development.
- According to a study, a 1% reduction in adult height as a result of childhood stunting is linked to a 1.4% reduction in economic productivity.
- Children who are stunted, earn 20% less as adults.
Malnutrition in North East India
- Upsurge in stunting: Four states in the Northeast Meghalaya, Mizoram, Nagaland and Tripura have seen an upsurge in stunting among children under the age of five. Stunting is highest in Meghalaya at 46.8 %, followed by Nagaland (32.7%), Tripura (32.3 %), and Mizoram (28.9%). In Mizoram, Nagaland, and Tripura, the percentage of kids who are stunted, wasting, underweight, or overweight has increased
- Levels of stunting decreased in Assam: The NFHS-5 shows Assam, Manipur and Sikkim have shown a drop in stunting levels. In Assam, stunting has decreased by almost one percentage point, although rates of overweight (2.3% to 4.9%), underweight (29.8% to 32.8%), and stunting (17% to 21.7%) have all increased, whereas that of wasting and underweight have decreased by more than 2% in each instance.
- Sikkim performs better than other NE states: As the number of stunted, wasting, and underweight children has dropped, Sikkim has done considerably better than other NE states so has Manipur, with a decrease in wasting from 6.8% to 9.9% in under-five children.
- Increase in no of overweight people in every NE state: Every state in the Northeast saw an increase in the number of overweight people, which amplifies the growing double burden of malnutrition in the states.
Appropriate foods and feeding practices show Higher immunity
- Feeding practices adequate only in Meghalaya and Tripura: The percentages of breastfeeding children receiving adequate complementary foods have improved only in Meghalaya and Tripura. Early initiation of breastfeeding is on the decline in six out of the eight northeastern states, with highest levels in Sikkim (33.5%) and Assam (15.3%).
- Reduction in exclusive breastfeeding rates (EBF): Sikkim, Tripura, and Manipur all exhibit a notable reduction in exclusive breastfeeding (EBF) rates. EBF in Sikkim is the lowest at 28.3 percent, far lower than the national average of 63.7 percent. Tripura demonstrated a gain of 39.5 percentage points in the practice of timely introduction of semi-solid food, whereas Meghalaya, Mizoram, Nagaland, Sikkim, and Arunachal Pradesh showed a slight fall.
- All NE states except Assam performed well on diet adequacy: Minimum Adequate Diet (or diet adequacy) is a combined indicator of feeding frequency and diet variety. From 8% to 29.8%, there is a significant range throughout the northeastern states. All states, with the exception of Assam, have performed better on this measure than the nation as a whole.
- The situation with obesity is more complicated: Only Meghalaya and Nagaland have seen decreases, while the other six states have seen increases. It is heartening to see a declining trend in underweight women (BMI < 18.5) in all eight northeastern states.
- Anaemia is increased: In six of the eight northeastern states, anaemia among women of reproductive age has increased, with Tripura worst at 67.2%, and Assam at 65.9%.
How malnutrition can be tackled in NE?
- Finding out the causes: Stunting among children in the Northeast is caused by a number of factors, including poor maternal health, a lack of antenatal care, inadequate infrastructure and healthcare facilities, inadequate feeding and nutrition for women, and limited access to education, clean drinking water, and sanitary facilities.
- For instance: Lack of toilets, drinking water and cooking fuels in the home environment have an impact on child malnutrition, according to a 2015 study on indigenous peoples in the Northeast.
- Improving the maternal nutrition: Manipur, Mizoram, and Sikkim fare better than the national average in most measures. Newborns’ chances of being stunted are decreased by better maternal nutrition prior to conception, throughout pregnancy, and after delivery. According to data for Sikkim, Manipur, and Mizoram, the risk of stunting decreases as the number of underweight mothers decreases.
- Upgrading the service availability: In the northeastern states, the use of supplementary food at the anganwadi centres (ANC) varies greatly, from about 35% in Arunachal Pradesh to 70% in Tripura. A low of 20.7% in Nagaland and a high of 79.4% in Manipur is the ANC coverage across the Northeast.
- Improving the required intake of Iron and Folic acid: All states have lower percentages of iron and folic acid (IFA) intake than the national average of 26%, with the exception of Manipur where 30.3% of pregnant women completed the full 180-day course of IFA tablets. Nagaland has the lowest rate, at just 4.1%. Overall, the NE states show a wide variation in service availability and uptake.
Note it down: The innovative programmes to enhance mother and child health
- Nutrition gardens: For example, the Assam government encouraged women in rural communities to develop “nutrition gardens” where they could grow vegetables.
- My school my Farm: “Kan Sikul, Kan Huan (My School, My Farm)” programme in the most impoverished and disaster-prone area in Mizoram-Lawngtlai.
- Lunchbox exchange: The “dibbi adaan pradaan (lunchbox exchange)” initiative in Hailakandi district of Assam for promoting better nutrition and variety in menu.
Conclusion
- Malnutrition in the Northeast has to be addressed holistically through the scaling up of direct nutrition interventions and the coupling of them with nutrition-sensitive measures to close the nutrition gap. In the long run, it could be beneficial to improve the monitoring and evaluation of current interventions by building on the POSHAN Abhiyaan and health projects.
Mains question
Q. What is Malnutrition? Malnutrition in the North-eastern states of India is worse than the country average. Discuss.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Status of Maternal mortality in India
From UPSC perspective, the following things are important :
Prelims level: MMR and recent figures
Mains level: Maternal mortality in India
Context
- India has improved its maternal mortality ratio (MMR) to 97 deaths per lakh in 2018-2020 from 103 deaths per lakh in 2017-2019. This is a considerable improvement from the 130 deaths per lakh in 2014-2016, the latest data released by the office of the Registrar General of India showed.
What is maternal mortality?
- As per World Health Organization, Maternal death is the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.
Click and get your FREE Copy of CURRENT AFFAIRS Micro Notes
Maternal mortality ratio (MMR)
- Main indicator: Maternal mortality ratio is a Kay indicator maternal mortality ratio.
- Definition: The maternal mortality ratio (MMR) is defined as the number of maternal deaths during a given time period per 100,000 live births during the same time period.
- Shows risk of maternal death: It depicts the risk of maternal death relative to the number of live births and essentially captures the risk of death in a single pregnancy or a single live birth.
- SDG target: Target 3.1 of Sustainable Development Goals (SDG) set by the United Nations aims at reducing the global maternal mortality ratio to less than 70 per 100,000 live births.
Maternal mortality Ratio (MMR) in India: An overview of recent figures
- North eastern states show improvement: In 2014-2016, the north-eastern state’s MMR was at a dangerously high 237 deaths per one lakh live births. This has improved significantly over the years to 229 in 2015-2017, 215 in 2016-2018 and 205 in 2017-2019, showed the data released November 28, 2022.
- Southern states always better than national average: The southern state was always performing better than the national average and has almost consistently brought down even that figure from 46 in 2014-2016, 42 in 2015-2017, 43 in 2016-2018 and 30 in 2017-2019.
- Kerala the best performer: Kerala continues to remain the best performer, with a low MMR of 19 per one lakh live births.
- On regional level Assam improved but continues to have high MMR: On the regional level, Assam continues to have the highest MMR (195) but has improved its own performance over the years.
- Better performing states: Among the better-performing states with an MMR lower than 100, barring Kerala, are Maharashtra (33), Telangana (43), Andhra Pradesh (45) and Gujarat (57).
- Other states with high MMR: Madhya Pradesh (173), Uttar Pradesh (167), Chhattisgarh (137), Odisha (119), Bihar (118), Rajasthan (113), Haryana (110), Punjab (105) and West Bengal (105).
- Sates with high MMR mostly belongs to socioeconomically poor regions: Most of these states belong to the Empowered Action Group (EAG) a classification of socioeconomically poor regions on whom the country’s development depends.
The Statistics including Maternal Mortality Rate and lifetime risk
- Maternal mortality rate: It is the maternal deaths of women in the ages 15-49 per lakh of women in that age group.
- As defined by Registrar General of India: The Registrar General of India defines as “the probability that at least one woman of reproductive age (15-49 years) will die due to childbirth or puerperium (postpartum period), assuming that chance of death is uniformly distributed across the entire reproductive span.”
Maternal Mortality Ratio (MMR) v/s Maternal Mortality Rate
- Maternal Mortality Ratio (MMR): This is derived as the proportion of maternal deaths per 1,00,000 live births, reported under the Sample Registration System (SRS).
- Maternal Mortality Rate: This is calculated as maternal deaths of women in the ages 15-49 per lakh of women in that age group, reported under SRS.
Maternal mortality rate in India
- India’s maternal mortality rate is six.
- poor-performing states include Madhya Pradesh (15.3), Uttar Pradesh (14.3), Assam (12.1), Bihar (11) and Chhattisgarh (9.9).
- Kerala is the only state to achieve a maternal mortality rate of less than one, at 0.9.
- Other states in the leading category include Maharashtra (1.8), Telangana (2.3), Andhra Pradesh (2.4) and Tamil Nadu (2.7).
- The lifetime risk figures also show a similar trend, with Madhya Pradesh leading the way at 0.53 per cent, followed by Uttar Pradesh (0.50 per cent), Assam (0.42 per cent), Bihar (0.39 per cent) and Chhattisgarh (0.35 per cent).
- At the national level, the lifetime risk of maternal mortality stands at 0.21 per cent.
Conclusion
- India’s performance on the maternal mortality front has been improving consistently as the country achieves its national target of reducing MMR to below 100.But it still lags behind the UN-mandated Sustainable Development Goals target of an MMR equivalent to 70 deaths per 100,000 live births. The country has eight years to meet this benchmark by 2030. Other indicators assessing maternal health indicate large room for improvement.
Mains question
Q. What is Maternal mortality. What is the difference between Maternal mortality ratio (MMR) and Maternal mortality rate. Evaluate India’s progress in reducing MMR.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Measles outbreak: Need to accelerate Children Immunization program
From UPSC perspective, the following things are important :
Prelims level: Measles and other contagious diseases
Mains level: Measles outbreak, Immunization program and the concerns
Context
- A measles outbreak in Mumbai has raised concerns amongst the country’s public health authorities. The city has reported more than 200 cases in the past two months and at least 13 children have lost their lives.
Click and get your FREE Copy of CURRENT AFFAIRS Micro Notes
Measles: A memory shot
- Measles is a highly contagious viral disease.
- Measles is caused by a virus in the paramyxovirus family and it is normally passed through direct contact and through the air.
- The virus infects the respiratory tract, then spreads throughout the body.
- Measles is a human disease and is not known to occur in animals.
All you need to know about Measles
- Signs and symptoms include:
- The first sign of measles is usually a high fever, runny nose, a cough, red and watery eyes, and small white spots inside the cheeks can develop in the initial stage.
- The most serious complications include blindness, encephalitis, severe diarrhoea and related dehydration, ear infections, or severe respiratory infections such as pneumonia.
- Who is at risk?
- Unvaccinated young children are at highest risk of measles and its complications, including death.
- Unvaccinated pregnant women are also at risk.
- Any non-immune person (who has not been vaccinated or was vaccinated but did not develop immunity) can become infected.
- Transmission:
- Measles is one of the world’s most contagious diseases.
- It is spread by coughing and sneezing, close personal contact or direct contact with infected nasal or throat secretions.
- Treatment:
- No specific antiviral treatment exists for measles virus.
- Severe complications from measles can be reduced through supportive care that ensures good nutrition, adequate fluid intake and treatment of dehydration with WHO-recommended oral rehydration solution.
- All children diagnosed with measles should receive two doses of vitamin A supplements.
- Prevention:
- Routine measles vaccination for children, combined with mass immunization campaigns in countries with high case and death rates, are key public health strategies to reduce global measles deaths.
- The measles vaccine is often incorporated with rubella and/or mumps vaccines.
Reasons sought behind the sudden outbreak of Measles in India
- A backslide in the universal immunisation programme during the pandemic:
- By all accounts, the outbreak seems to have been precipitated by a backslide in the universal immunisation programme during the pandemic.
- According to the state government data, only 41 per cent of the eligible children have been inoculated against measles in Mumbai.
- Vaccine hesitancy:
- Parents, reportedly, are showing a disinclination to continue the inoculation regime for their children after they developed fever on being administered the first jab.
- Overworked public health professionals, including ASHA workers, have also had to combat vaccine hesitancy.
Government efforts and the status of Immunization programs
- Mission Indradhanush: In recent years, the Centre’s Mission Indradhanush project has improved vaccine coverage and reduced delays between shots.
- Low coverage in last two years: WHO and UNICEF studies have shown that immunisation programmes especially those focusing on DPT (diphtheria, pertussis and tetanus) and measles have taken a hit in low- and mid-income countries, including India, in the past two years.
- Missed shots during Pandemic restrictions: Early in the pandemic, the National Health Mission’s information system reported that at least 100,000 children missed their shots because of the restrictions on movement.
- India speeding up the immunization after the pandemic: Anecdotal reports do indicate that India’s universal inoculation programme picked up during the latter part of the pandemic. But measles is a highly contagious disease. Experts had cautioned that even a 5 per cent fall in the vaccination rate can disrupt herd immunity and precipitate an outbreak. The surge of the disease in Mumbai indicates that their fears are coming true.
Countries with lower per capita incomes are more at risk
- Measles is still common in many developing countries particularly in parts of Africa and Asia. The overwhelming majority (more than 95%) of measles deaths occur in countries with low per capita incomes and weak health infrastructures.
- Measles outbreaks can be particularly deadly in countries experiencing or recovering from a natural disaster or conflict. Damage to health infrastructure and health services interrupts routine immunization, and overcrowding in residential camps greatly increases the risk of infection.
- Measles outbreaks can result in epidemics that cause many deaths, especially among young, malnourished children. In countries where measles has been largely eliminated, cases imported from other countries remain an important source of infection.
Conclusion
- Studies have shown that child vaccination had suffered during the pandemic as attention shifted towards adult vaccination. Now that the pandemic has waned, governments must carefully evaluate at the grassroots how many children fell out of the vaccine net during this period and take countermeasures.
Mains question
Q. Measles is a highly contagious disease with a high mortality rate in unvaccinated children. Discuss the reasons behind the recent outbreak of measles in India.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
All women have Right to Legal and Safe Abortion: Supreme Court
From UPSC perspective, the following things are important :
Prelims level: MRTP Act
Mains level: Abortion rights debate
The Supreme Court has held that all women, irrespective of their marital status, are entitled to safe and legal abortion till 24 weeks of pregnancy under the Medical Termination of Pregnancy (MTP) Act.
A case for safe abortion
- A Bench led by Justice D.Y. Chandrachud was hearing the appeal of a woman who wanted to abort her 24-week pregnancy after her relationship failed and her partner left her.
- The lower court had taken an “unduly restrictive view” that her plea for a safe abortion was not covered under the Medical Termination of Pregnancy Act.
- This was since the pregnancy arose from a consensual relationship outside wedlock.
What was the last amendment?
- The court noted that an amendment to the Act in 2021 had substituted the term ‘husband’ with ‘partner’, a clear signal that the law covered unmarried women within its ambit.
Reiterating the live-in recognition
- Chastising the lower court, the Bench said live-in relationships had already been recognised by the Supreme Court.
- There were a significant number of people in social mainstream who see no wrong in engaging in pre-marital sex.
- The law could not be used to quench “notions of social morality” and unduly interfere in their personal autonomy and bodily integrity.
About Medical Termination of Pregnancy (MTP) Act
- Abortion in India has been a legal right under various circumstances for the last 50 years since the introduction of the Medical Termination of Pregnancy (MTP) Act in 1971.
- The Act was amended in 2003 to enable women’s access to safe and legal abortion services.
- Abortion is covered 100% by the government’s public national health insurance funds, Ayushman Bharat and Employees’ State Insurance with the package rate for surgical abortion.
The idea of terminating your pregnancy cannot originate by choice and is purely circumstantial. There are four situations under which a legal abortion is performed:
- If continuation of the pregnancy poses any risks to the life of the mother or mental health
- If the foetus has any severe abnormalities
- If pregnancy occurred as a result of failure of contraception (but this is only applicable to married women)
- If pregnancy is a result of sexual assault or rape
The pregnancy can be terminated upto 24 weeks of gestational age after the opinion of two registered medical practitioners under these conditions —
- If the woman is either a survivor of sexual assault or rape or incest
- If she is a minor
- If her marital status has changed during the ongoing pregnancy (i.e. either widowhood or divorce)
- If she has major physical disabilities or is mentally ill
- On the grounds of foetal malformation incompatible with life or if the child is born, it would be seriously handicapped
- If the woman is in humanitarian settings or disaster, or emergency situations as declared by the government
These are the key changes that the Medical Termination of Pregnancy (Amendment) Act, 2021, has brought in:
- The gestation limit for abortions has been raised from the earlier ceiling of 20 weeks to 24 weeks, but only for special categories of pregnant women such as rape or incest survivors. But this termination would need the approval of two registered doctors.
- All pregnancies up to 20 weeks require one doctor’s approval. The earlier law, the MTP Act 1971, required one doctor’s approval for pregnancies upto 12 weeks and two doctors’ for pregnancies between 12 and 20 weeks.
- Women can now terminate unwanted pregnancies caused by contraceptive failure, regardless of their marital status. Earlier the law specified that only a “married woman and her husband” could do this.
- There is also no upper gestation limit for abortion in case of foetal disability if so decided by a medical board of specialist doctors, which state governments and union territories’ administrations would set up.
Criticism of Abortion
- Foetuses feel the pain: If the foetus is beyond 20 weeks of gestation, gynaecs assume that there will be pain caused to the foetus.
- Abortions cause psychological damage: Young adult women who undergo abortion may be at increased risk for subsequent depression.
- Abortions reduce the number of adoptable babies: Instead of having the option to abort, women should give their unwanted babies to people who cannot conceive. Single parenthood is also gaining popularity in the US.
- Cases of selective abortion: Such cases based on physical and genetic abnormalities (eugenic termination) is overt discrimination.
- Abortion as a form of contraception: It is immoral to kill an unborn child for convenience. Many women are using abortion as a contraceptive method.
- Morality put to question: If women become pregnant, they should accept the responsibility that comes with producing a child. People need to take responsibility for their actions and accept the consequences.
- Abortion promotes throwaway culture: The legalization of abortion sends a message that human life has little value and promotes the throwaway culture.
Arguments in favour for Abortion Rights
- Upholding individual conscience and decision-making: The US Supreme Court has declared abortion to be a fundamental right guaranteed by the US Constitution.
- Reproductive choice empowers women: The choice over when and whether to have children is central to a woman’s independence and ability to determine her future.
- Foetal viability occurs post-birth: Personhood begins after a foetus becomes “viable” (able to survive outside the womb) or after birth, not at conception. Abortion is the termination of a pregnancy, not a baby.
- No proof of foetal pain: Most neuroscientists believe that the cortex is necessary for pain perception. The cortex does not become functional until at least the 26th week of a foetus’ development.
- Preventing illegal abortions: Access to legal, professionally-performed abortions reduces maternal injury and death caused by unsafe, illegal abortions.
- Mother’s health: Modern abortion procedures are safe and do not cause lasting health issues such as cancer and infertility.
- Child’s health: Abortion gives pregnant women the option to choose not to bring fetuses with profound abnormalities to full term.
- Prevents women’s exclusion: Women who are denied abortions are more likely to become unemployed, to be on public welfare, to be below the poverty line, and to become victims of domestic violence.
- Reproductive choice protects women from financial disadvantage: Many women who choose abortion don’t have the financial resources to support a child.
- Justified means of population control: Many defends abortion as a way to curb overpopulation. Malnutrition, starvation, poverty, lack of medical and educational services, pollution, underdevelopment, and conflict over resources are all consequences of overpopulation.
Conclusion
- Hence it is now established that the right to abortion is a legal right of all women.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
How lower fertility rate hampers demographic dividend in number of ways
From UPSC perspective, the following things are important :
Prelims level: NA
Mains level: human population
 Context
Context
- Though the Global population, in terms of numbers, has been steadily increasing the average global fertility rate has been consistently declining over the past 70 years.
What Reports say?
- Reports suggest that the global population could grow to around 8.5 billion in 2030.
- According to the World Population Prospects 2022, Average number of children per woman in the reproductive age group has declined by 50%, from an average of five children per woman in 1951 to4 children in 2020.
What is Fertility?
- Fertility is the quality or state of being fertile.
- Fertility is the ability to reproduce through normal sexual interaction. In other words it is the natural capacity to conceive a biological child.
- Fertilitychanges with age. Both males and females become fertile in their teens following puberty.
 What is fertility rate?
What is fertility rate?
- The number of live births in women over a specific length of time.
- Total fertility rate is the average number of children born to a woman during her lifetime.
Recent findings
The newly released World Population Prospectus notes that the global fertility rate fell from three in 1990 to 2.3 in 2021.
Overview of fertility dynamics
- Reason: Speeding up the social phenomenon of demographic transition.
- Poorer countries: speeding up the Transition a lot faster than the richer ones.
- Britain: Took 130 years to transition from a fertility rate of five per woman in 1800 to two in 1930, whereas
- South Korea: Took 20 years from 1965 to 1985 to achieve the same. South Korea reporting the lowest fertility rate, 1.05 children per woman.
- Most advanced economies: Have their fertility rate below the replacement rate of 2.1.
- Sub-Saharan African countries: Expected to contribute more than half the population growth after 2050 and grow through 2100. For example, Niger a sub Saharan country with highest fertility rate in the world, estimated to be 91 children per woman.
- What is Demographic transition: is a long-term trend of declining birth and death rate. It is shift from high birth rates to low birth rates in societies with minimal technology, education (especially of women) and economic development and from high death rates to Low death rates in societies with advanced economies and development.

Where India Stands
- According to National Family Health Survey (NFHS), fertility rate falling below the replacement level for the first time to 2.0 in 2021.dropped from 2.2 to 2.0.
- only five States have a fertility rate above the replacement rate: Bihar (3), Meghalaya (2.9), Uttar Pradesh (2.4), Jharkhand (2.3), and Manipur (2.2)
- At the time of Independence, India’s fertility rate was six per woman, and it had taken 25 years to reach five, with the government launching the first ever family planning program in the world in 1952.
- India’s fertility further declined to four in the 1990s when Kerala became the first State in India to have a fertility rate below replacement l
- Increased use of contraception, more years of average schooling, better health care, and an increase in the mean marriage age of women are of the reasons behind the steady dip in fertility rate.
Lower fertility rate as cause and consequences on the economy
Positive impact:
- Lower fertility leads to rise in women’s education.
- Window of time where the ration of working-age population is higher than that of the dependent age groups.
- This high proportion of people in the workforce boosts income and investment, and higher level of saving.
- Lower pressure on land, water and other resources and would also contribute to achieving environmental goals.
- Advanced health care and better nutrition, results in increased life expectancy and productivity of citizens.
Negative impact:
- Lower fertility impacts women’s education positively, which in turn lowers the fertility of the next generations.
- While the income rises with better health care and better infrastructure development, Fertility drops.
- A fall in fertility rate beyond replacement level would have a negative effect on the proportion of the working population, which in turn will affect output in an economy.
- After the window of demographic dividend, the huge working age population moves to old age, supported by fewer workers.
- Japan was the first country to experience the implications of falling fertility rates. Country is now facing fiscal challenges to meet rising social security costs.
Experiments to deal with fertility decline
Countries across the globe are experimenting with policies to boost fertility.
- Germany: found success in boosting births through liberal labour laws, allowing more parental leave and benefits.
- Denmark: offering state-funded IVF for women below 40 years
- Hungary: Recently nationalized IVF clinics.
- Poland: Gives out monthly cash payments to parents having more than two children
- Russia: Makes one-time payment to parents when their second child is born. Reinstituted the Soviet-era ‘Mother Heroine’ title, who bore and raised more than 10 children amounting to almost a one-time payment of 13 lakh.
Way ahead
- Need of the hour is to ensure liberal labor reforms, encourage higher female labor force participation, higher focus on nutrition and health.
- Although India’s working age population will continue to grow for many more decades, it would need to keep an eye on fertility dips.
Mains Question
What are Implications of lower fertility rate on the economy? What steps could be taken to deal with fertility decline? Discuss.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Panel moots district-level survey to bring more children into adoption ambit
From UPSC perspective, the following things are important :
Prelims level: CARA
Mains level: Child Adoption
A report recently tabled on “Review of Guardianship and Adoption Laws” in Parliament has stated that- India despite a country with millions of orphans, there are only 2,430 children available for adoption.
What is the news?
- There are many enthusiastic parents who are ready to adopt children.
- To address this paradox, a Parliamentary panel has recommended district-level surveys to proactively identify orphaned and abandoned children.
- According to the report, there were 27,939 prospective parents registered with the Child Adoption Resource Authority (CARA) as on December 2021, up from nearly 18,000 in 2017.
What is CARA?
- Central Adoption Resource Authority (CARA) is an autonomous and statutory body of the Ministry of Women and Child Development. It was set up in 1990.
- It functions as the nodal body for the adoption of Indian children and is mandated to monitor and regulate in-country and inter-country adoptions.
- CARA is designated as the Central Authority to deal with inter-country adoptions in accordance with the provisions of the 1993 Hague Convention on Inter-country Adoption, ratified India in 2003.
- It primarily deals with the adoption of orphaned, abandoned and surrendered children through its associated and recognized adoption agencies.
Adoption Process
- The eligibility of prospective adoptive parents living in India, duly registered on the Child Adoption Resource Information and Guidance System (CARINGS), irrespective of marital status and religion, is Procedure for adoption adjudged by specialised adoption agencies preparing home study reports.
- The specialized adoption agency then secures court orders approving the adoption.
- All non-resident persons approach authorized adoption agencies in their foreign country of residence for registration under CARINGS.
- Their eligibility is adjudged by authorised foreign adoption agencies through home study reports.
- CARA then issues a pre-adoption ‘no objection’ certificate for foster care, followed by a court adoption order.
- A final ‘no objection’ certificate from CARA or a conformity certificate under the adoption convention is mandatory for a passport and visa to leave India.
What else regulates child adoption?
- The Juvenile Justice (Care and Protection of Children) Act, 2015 permits the adoption of same-sex children, allowing biological or adopted parents to adopt a child of the same gender.
- A single or divorced person can adopt under the JJ Act, but a single male cannot adopt a girl child.
- According the Hindu Adoption and Maintenance Act, 1956 (HAMA), a Hindu parent or guardian can place a child for adoption with another Hindu parent under the Act.
- A prospective parent can also adopt a male child if he has no other male children or grandchildren, or a female child if he has no other female children or grandchildren.
Issues with child adoption in India
- Parent-centrism: The current adoption approach is very parent-centred, but parents must make it child-centred.
- Age of child: Most Indian parents also want a child between the ages of zero and two, believing that this is when the parent-child bond is formed.
- Institutional issues: Because the ratio of abandoned children to children in institutionalised care is lopsided, there are not enough children available for adoption.
- Lineage discrimination: Most Indians have a distorted view of adoption because they want their genes, blood, and lineage to be passed down to their children.
- Red-tapism: Child adoption is also not so easy task after the Juvenile Justice Rules of 2016 and the Adoption Regulations of 2017 were launched.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Replacement Level Fertility achieved in India
From UPSC perspective, the following things are important :
Prelims level: RLF
Mains level: Population stabilization in India
India has achieved replacement level fertility, with 31 States and UTs reaching a Total Fertility Rate (an average number of children per woman) of 2.1 or less, Union Minister of State for Health and Family Welfare has informed Parliament.
What is Replacement Level Fertility?
- Replacement level fertility is the level of fertility at which a population exactly replaces itself from one generation to the next.
- In simpler terms, it denotes the fertility number required to maintain the same population number of a country over a given period of time.
- In developed countries, replacement level fertility can be taken as requiring an average of 2.1 children per woman.
- In countries with high infant and child mortality rates, however, the average number of births may need to be much higher.
- RLF will lead to zero population growth only if mortality rates remain constant and migration has no effect.
Benefits of achieving RLF
- RLF helps ensure greater food security.
- The reduced demand for food would in turn lessen agri- culture’s impact on the environment.
- It would also likely lead to economic benefits through a “demographic dividend.”
- Finally, achieving replacement level fertility would yield significant social benefits―especially for women.
How did India achieve this?
- Between 2012 and 2020, the country added more than 1.5 crore additional users for modern contraceptives, thereby increasing their use substantially.
- India has witnessed a paradigm shift from the concept of population control to population stabilisation to interventions being embedded toward ensuring harmony of continuum care.
Way forward
- Although India has achieved replacement level fertility, there is still a significant population in the reproductive age group that must remain at the centre of our intervention efforts.
- India’s focus has traditionally been on the supply side, the providers and delivery systems but now it’s time to focus on the demand side which includes family, community and society.
- Significant change is possible with this focus, instead of an incremental change.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Rise in Unvaccinated Children in India
From UPSC perspective, the following things are important :
Prelims level: Mission Indradhanush
Mains level: Read the attached story
The number of children in India who were unvaccinated or missed their first dose of diphtheria-tetanus-pertussis (DTP) combined vaccine doubled due to the pandemic, rising from 1.4 million in 2019 to 2.7 million in 2021, according to official data published by the WHO and UNICEF.
Why in news?
- This data signifies that the world recorded the largest sustained decline in childhood vaccinations in approximately 30 years.
- There was an increase in zero dose.
- This is the first time ever there has been a decline in evaluated coverage in immunisation for India as a whole.
Vaccination measures in India
- Intensified Mission Indradhanush (IMI) 4.0: India started IMI 4.0 from February 2022, which is expected to further reduce the number of unvaccinated children.
- India’s Universal Immunisation Programme (UIP): It provide free vaccines to all children across the country to protect them against Tuberculosis, Diphtheria, Pertussis, Tetanus, Polio, Hepatitis B, Pneumonia and Meningitis due to Haemophilus Influenzae type b (Hib), Measles, Rubella, Japanese Encephalitis (JE) and Rotavirus diarrhoea. (Rubella, JE and Rotavirus vaccine in select states and districts).
About Intensified Mission Indhradhanush (IMI) 4.0
- IMI 4.0 aims to fill gaps in the routine immunisation coverage of infants and pregnant women hit by the Covid-19 pandemic and also aims to make lasting gains towards Universal Immunization.
- It will have three rounds and will be conducted in 416 districts across 33 states.
- Unlike the past, each round under IMI 4.0 will be conducted for seven days, including Routine Immunization (RI) days, Sundays, and public holidays.
Mission Indradhanush (MI)
|
Back2Basics: Universal Immunisation Programme
- The Expanded Programme on Immunization was launched in 1978.
- It was renamed as UIP in 1985 when its reach was expanded beyond urban areas.
- UIP is one of the largest public health programmes targeting close to 2.67 crore newborns and 2.9 crore pregnant women annually.
- Under UIP, Immunization is provided free of cost against 12 vaccine-preventable diseases.
- The two major milestones of UIP have been the elimination of polio in 2014 and maternal and neonatal tetanus elimination in 2015.
- To speed up the coverage, Mission Indradhanush was planned and implemented to rapidly increase the full coverage to 90%.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Malnutrition in India
From UPSC perspective, the following things are important :
Prelims level: National Nutrition Mission
Mains level: Paper 2- Need for direct nutrition intervention
Context
More than seven decades after independence, India still suffers from the public health issues such as child malnutrition attributing to 68.2% of under-five child mortality.
What is malnutrition?
- Malnutrition refers to deficiencies, excesses or imbalances in a person’s intake of energy and/or nutrients.
- The term malnutrition covers 2 broad groups of conditions.
- One is ‘undernutrition’—which includes stunting (low height for age), wasting (low weight for height), underweight (low weight for age) and micronutrient deficiencies or insufficiencies (a lack of important vitamins and minerals).
- The other is overweight, obesity and diet-related non-communicable diseases (such as heart disease, stroke, diabetes, and cancer).
Marginal improvement on Stunting and Wasting
- The National Family Health Survey (NFHS-5) has shown marginal improvement in different nutrition indicators, indicating that the pace of progress is slow.
- This is despite declining rates of poverty, increased self-sufficiency in food production, and the implementation of a range of government programmes.
- Children in several States are more undernourished now than they were five years ago.
- Increased stunting in some states: Stunting is defined as low height-for-age.
- While there was some reduction in stunting rates (35.5% from 38.4% in NFHS-4) 13 States or Union Territories have seen an increase in stunted children since NFHS-4.
- This includes Gujarat, Maharashtra, West Bengal and Kerala.
- Wasting remains stagnant: Wasting is defined as low weight-for-height.
- Malnutrition trends across NFHS surveys show that wasting, the most visible and life-threatening form of malnutrition, has either risen or has remained stagnant over the years.
National Nutrition Mission (NNM): Focus on essential nutrition interventions
- Government appears determined to set it right — with an aggressive push to the National Nutrition Mission (NNM), rebranding it the Prime Minister’s Overarching Scheme for Holistic Nutrition, or POSHAN.
- Window of opportunity: The Ministry of Women and Child (MWCD) continues to be the nodal Ministry implementing the NNM with a vision to align different ministries to work in tandem on the “window of opportunity” of the first 1,000 days in life (270 days of pregnancy and 730 days; 0-24 months).
- POSHAN Abhiyaan (now referred as POSHAN 2.0) rightly places a special emphasis on selected high impact essential nutrition interventions, combined with nutrition-sensitive interventions, which indirectly impact mother, infant and young child nutrition, such as improving coverage of maternal-child health services, enhancing women empowerment, availability, and access to improved water, sanitation, and hygiene and enhancing homestead food production for a diversified diet.
Key findings of NHFS-5 data
- Data from the National Family Health Survey (NFHS)-5 2019-21, as compared to NFHS-4 2015-16, reveals a substantial improvement in a period of four to five years in several proxy indicators of women’s empowerment.
- No progress on nutritional intervention: Alarmingly, during this period, the country has not progressed well in terms of direct nutrition interventions.
- Preconception nutrition, maternal nutrition, and appropriate infant and child feeding remain to be effectively addressed.
- India has 20% to 30% undernutrition even in the first six months of life when exclusive breastfeeding is the only nourishment required.
- Neither maternal nutrition care interventions nor infant and young child feeding practices have shown the desired improvement.
Suggestions
- Child undernutrition in the first three months remains high. Creating awareness on EBF, promoting the technique of appropriate holding, latching and manually emptying the breast are crucial for the optimal transfer of breast milk to a baby.
- Complementary feeding: NFHS-5 also confirms a gap in another nutrition intervention — complementary feeding practices, i.e., complementing semi-solid feeding with continuation of breast milk from six months onwards.
- The fact that 20% of children in higher socio- economic groups are also stunted indicates poor knowledge in food selection and feeding practices and a child’s ability to swallow mashed feed.
- Creating awareness: So, creating awareness at the right time with the right tools and techniques regarding special care in the first 1,000 days deserves very high priority.
- Revisit nodal system for nutrition program: There is a need to revisit the nodal system for nutrition programme existing since 1975, the Integrated Child Development Scheme (ICDS) under the Ministry of Women and Child and examine whether it is the right system for reaching mother-child in the first 1000 days of life.
- Alternative way to distribute ICDS supplies: There is also a need to explore whether there is an alternative way to distribute the ICDS supplied supplementary nutrition as Take- Home Ration packets through the Public Distribution (PDS) and free the anganwadi workers of the ICDS to undertake timely counselling on appropriate maternal and child feeding practices.
Conclusion
It is time to think out of the box, and overcome systemic flaws and our dependence on the antiquated system of the 1970s that is slowing down the processes.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Is India really ahead of the West in terms of reproductive rights?
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2- Reproductive rights in India
Context
Contrary to the grandstanding since the overturning of the landmark Roe V. Wade judgment, the truth is that India is not ahead of the West in terms of reproductive rights.
Medical Termination of Pregnancy (MTP) Act
- Abortion in India has been a legal right under various circumstances for the last 50 years with the introduction of Medical Termination of Pregnancy (MTP) Act in 1971.
- The Act was amended in 2003 to enable women’s accessibility to safe and legal abortion services.
- Abortion is covered 100% by the government’s public national health insurance funds, Ayushman Bharat and Employees’ State Insurance with the package rate for surgical abortion.
The idea of terminating your pregnancy cannot originate by choice and is purely circumstantial. There are four situations under which a legal abortion is performed:
- If continuation of the pregnancy poses any risks to the life of the mother or mental health
- If the foetus has any severe abnormalities
- If pregnancy occurred as a result of failure of contraception (but this is only applicable to married women)
- If pregnancy is a result of sexual assault or rape
These are the key changes that the Medical Termination of Pregnancy (Amendment) Act, 2021, has brought in:
- The gestation limit for abortions has been raised from the earlier ceiling of 20 weeks to 24 weeks, but only for special categories of pregnant women such as rape or incest survivors. But this termination would need the approval of two registered doctors.
- All pregnancies up to 20 weeks require one doctor’s approval. The earlier law, the MTP Act 1971, required one doctor’s approval for pregnancies upto 12 weeks and two doctors’ for pregnancies between 12 and 20 weeks.
- Women can now terminate unwanted pregnancies caused by contraceptive failure, regardless of their marital status. Earlier the law specified that only a “married woman and her husband” could do this.
- There is also no upper gestation limit for abortion in case of foetal disability if so decided by a medical board of specialist doctors, which state governments and union territories’ administrations would set up.
Issues with legal provisions related to reproductive rights in India
- Lack of rights based approach: The Medical Termination of Pregnancy (Amendment) Act 2021 is far from ideal and has been criticised for not taking a rights-based approach.
- According to the Act, a pregnancy can be terminated on the following conditions: Grave danger to the physical/mental health of the pregnant woman; foetal abnormalities; rape/coercion; and contraceptive failure.
- A woman’s right to choose to end the pregnancy even in the first few weeks is still not recognised in India.
- Systemic barriers: It doesn’t give the pregnant person complete autonomy in ending the pregnancy, instead making them go through various systemic barriers.
- The final decision falls not on the pregnant person, but on registered medical practitioners (RMP).
- The constitution of a medical board, a requirement by the Act, is considered a barrier by the World Health Organisation.
- Excludes transgenders and non-binary persons: Additionally, it uses the word “woman”, thereby leaving out pregnant transgender and non-binary persons who are biologically capable of bearing children.
- It forces them to identify themselves in the gender-binary ignoring their gender identity.
Social factors and lack of medical facilities
- It is important to look through an intersectional lens, and factor in class and caste privilege.
- Abortion facilities in private medical centres are expensive, available only for those who have the resources.
- Lack of access: Not all public health centres, especially in rural India, provide abortion facilities.
- Most unmarried women end up resorting to unsafe abortions in illegal clinics or at home.
- According to the latest National Family Health Survey 2019-2021, 27 percent of the abortions were carried out by the woman herself at home.
- According to United Nations’ Population Fund’s (UNFPA) State of the World Population Report 2022, around 8 women die each day in India due to unsafe abortions.
- It also found that between 2007-2011, 67 percent of the abortions were classified as unsafe.
- Unsafe abortion was one of the top three causes of maternal deaths.
Discussion on reproductive rights in India are incomplete without mentioning surrogacy.
Issues in the Surrogacy (Regulation) Act 2021
- While well-intentioned, leaves much to be desired.
- The plethora of regulations one must undergo is antithetical to a dignified standard of living.
- Exclusionary in nature: Experts have pointed out that the Act is exclusionary in nature, disregards privacy, and also exploits women’s reproductive labour.
- Only a heterosexual married couple (with certain preconditions) can be the intending parents.
- It strips the reproductive autonomy of LGBTQ+ persons and single, divorced, and widowed intending parents. It can be seen as a violation to the fundamental right to equality.
- Experts also believe that regulations, rather than a complete ban on commercial surrogacy, should have been the way forward.
- Violates right to privacy: The Act requires the intending couple to declare their infertility and reveals the identity of the surrogate, both of which violate the right to privacy.
- The landmark Puttaswamy judgment discusses bodily privacy – the right over one’s body and “the freedom of being able to prevent others from violating one’s body.”
- The current reproductive rights regulatory framework falls short in guaranteeing bodily privacy.
Conclusion
The situation in India is far from perfect and we should take this moment to reflect and learn from progressive practices around the world. We should strive for inclusivity, complete bodily autonomy, and reproductive equity.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
US Supreme Court overturns Abortion Right
From UPSC perspective, the following things are important :
Prelims level: MRTP Act
Mains level: Abortion rights debate
In a significant curtailment of women’s rights, the US Supreme Court overturned Roe v. Wade, a 1973 landmark decision giving women in America the right to have an abortion before the foetus is viable outside the womb — before the 24-28 week mark.
What is Roe vs. Wade Case: Upholding the Right to Abortion
- Roe, short for Jane Roe, is the pseudonym for a Texas woman who in 1970 sought to have an abortion when she was five months pregnant.
- Texas then had ban on abortions except to save a mother’s life. The case then went to the US Supreme Court (SCOTUS).
- The 7-2 majority opinion of the SCOTUS written in 1973, paved the way for the recognition of abortion as a constitutional right in the US considering foetal viability.
[Foetal viability is the point at which a foetus can survive outside the womb, at the time considered to be around 28 weeks, but today is closer to 23 or 24 weeks owing to advances in medicine and technology.]
Right to Abortion Judgment: Key takeaways
Based on the Roe vs Wade case, the framework of regulations that applied towards the right to abortion:
- Almost no limitations could be placed on that right;
- Only limitations to abortion rights that were aimed at protecting a woman’s health were permitted; and in the third trimester,
- State governments had greater leeway to limit the right to abortion except for cases in which the life and health of the mother were endangered.
What is the debate?
The abortion debate is the ongoing controversy surrounding the moral, legal, and religious status of induced abortion.
The sides involved in the debate are the self-described “pro-choice” and “pro-life” movements.
- Pro-choice emphasizes the woman’s choice whether to terminate a pregnancy.
- Pro-life position stresses the humanity of both the mother and foetus, arguing that a fetus is a human person deserving of legal protection.
Why is the judgement overturned?
- Foetuses feel the pain: If the foetus is beyond 20 weeks of gestation, gynaecs assume that there will be pain caused to the foetus.
- Biblical gospel: The Bible does not draw a distinction between foetuses and babies. By the time a baby is conceived, he or she is recognized by God.
- Abortions cause psychological damage: Young adult women who undergo abortion may be at increased risk for subsequent depression.
- Abortions reduce the number of adoptable babies: Instead of having the option to abort, women should give their unwanted babies to people who cannot conceive. Single parenthood is also gaining popularity in the US.
- Cases of selective abortion: Such cases based on physical and genetic abnormalities (eugenic termination) is overt discrimination.
- Abortion as a form of contraception: It is immoral to kill an unborn child for convenience. Many women are using abortion as a contraceptive method.
- Morality put to question: If women become pregnant, they should accept the responsibility that comes with producing a child. People need to take responsibility for their actions and accept the consequences.
- Abortion promotes throwaway culture: The legalization of abortion sends a message that human life has little value and promotes the throwaway culture.
- Racial afflictions: Abortion disproportionately affects African American babies. In the US, black women are 3.3 times as likely as white women to have an abortion.
Arguments in favour for Abortion Rights
- Upholding individual conscience and decision-making: The US Supreme Court has declared abortion to be a fundamental right guaranteed by the US Constitution.
- Reproductive choice empowers women: The choice over when and whether to have children is central to a woman’s independence and ability to determine her future.
- Foetal viability occurs post-birth: Personhood begins after a foetus becomes “viable” (able to survive outside the womb) or after birth, not at conception. Abortion is the termination of a pregnancy, not a baby.
- No proof of foetal pain: Most neuroscientists believe that the cortex is necessary for pain perception. The cortex does not become functional until at least the 26th week of a foetus’ development.
- Preventing illegal abortions: Access to legal, professionally-performed abortions reduces maternal injury and death caused by unsafe, illegal abortions.
- Mother’s health: Modern abortion procedures are safe and do not cause lasting health issues such as cancer and infertility.
- Child’s health: Abortion gives pregnant women the option to choose not to bring fetuses with profound abnormalities to full term.
- Prevents women’s exclusion: Women who are denied abortions are more likely to become unemployed, to be on public welfare, to be below the poverty line, and to become victims of domestic violence.
- Reproductive choice protects women from financial disadvantage: Many women who choose abortion don’t have the financial resources to support a child.
- Justified means of population control: Many defends abortion as a way to curb overpopulation. Malnutrition, starvation, poverty, lack of medical and educational services, pollution, underdevelopment, and conflict over resources are all consequences of overpopulation.
Way forward
- A search for the middle path perhaps the right of a woman to choose what to do with the foetus has to be balanced with the right of the foetus to survive.
- It is only that a foetus does not have the ability to exercise an option while the person who carries it does.
- Rather than banning abortion, lawmakers must focus on counselling, employment security, social welfare, and financial support to persuade pregnant women to give birth to their children.
- We must achieve some degree of protection for the unborn by obtaining voluntary recognition of personal responsibility and respect for the personhood of the unborn.
Back2Basics: Medical Termination of Pregnancy (MTP) Act
- Abortion in India has been a legal right under various circumstances for the last 50 years with the introduction of Medical Termination of Pregnancy (MTP) Act in 1971.
- The Act was amended in 2003 to enable women’s accessibility to safe and legal abortion services.
- Abortion is covered 100% by the government’s public national health insurance funds, Ayushman Bharat and Employees’ State Insurance with the package rate for surgical abortion.
The idea of terminating your pregnancy cannot originate by choice and is purely circumstantial. There are four situations under which a legal abortion is performed:
- If continuation of the pregnancy poses any risks to the life of the mother or mental health
- If the foetus has any severe abnormalities
- If pregnancy occurred as a result of failure of contraception (but this is only applicable to married women)
- If pregnancy is a result of sexual assault or rape
These are the key changes that the Medical Termination of Pregnancy (Amendment) Act, 2021, has brought in:
- The gestation limit for abortions has been raised from the earlier ceiling of 20 weeks to 24 weeks, but only for special categories of pregnant women such as rape or incest survivors. But this termination would need the approval of two registered doctors.
- All pregnancies up to 20 weeks require one doctor’s approval. The earlier law, the MTP Act 1971, required one doctor’s approval for pregnancies upto 12 weeks and two doctors’ for pregnancies between 12 and 20 weeks.
- Women can now terminate unwanted pregnancies caused by contraceptive failure, regardless of their marital status. Earlier the law specified that only a “married woman and her husband” could do this.
- There is also no upper gestation limit for abortion in case of foetal disability if so decided by a medical board of specialist doctors, which state governments and union territories’ administrations would set up.
UPSC 2023 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Maternal Mortality in India
From UPSC perspective, the following things are important :
Prelims level: Maternal Mortality , key trends
Mains level: Institutional birth in India
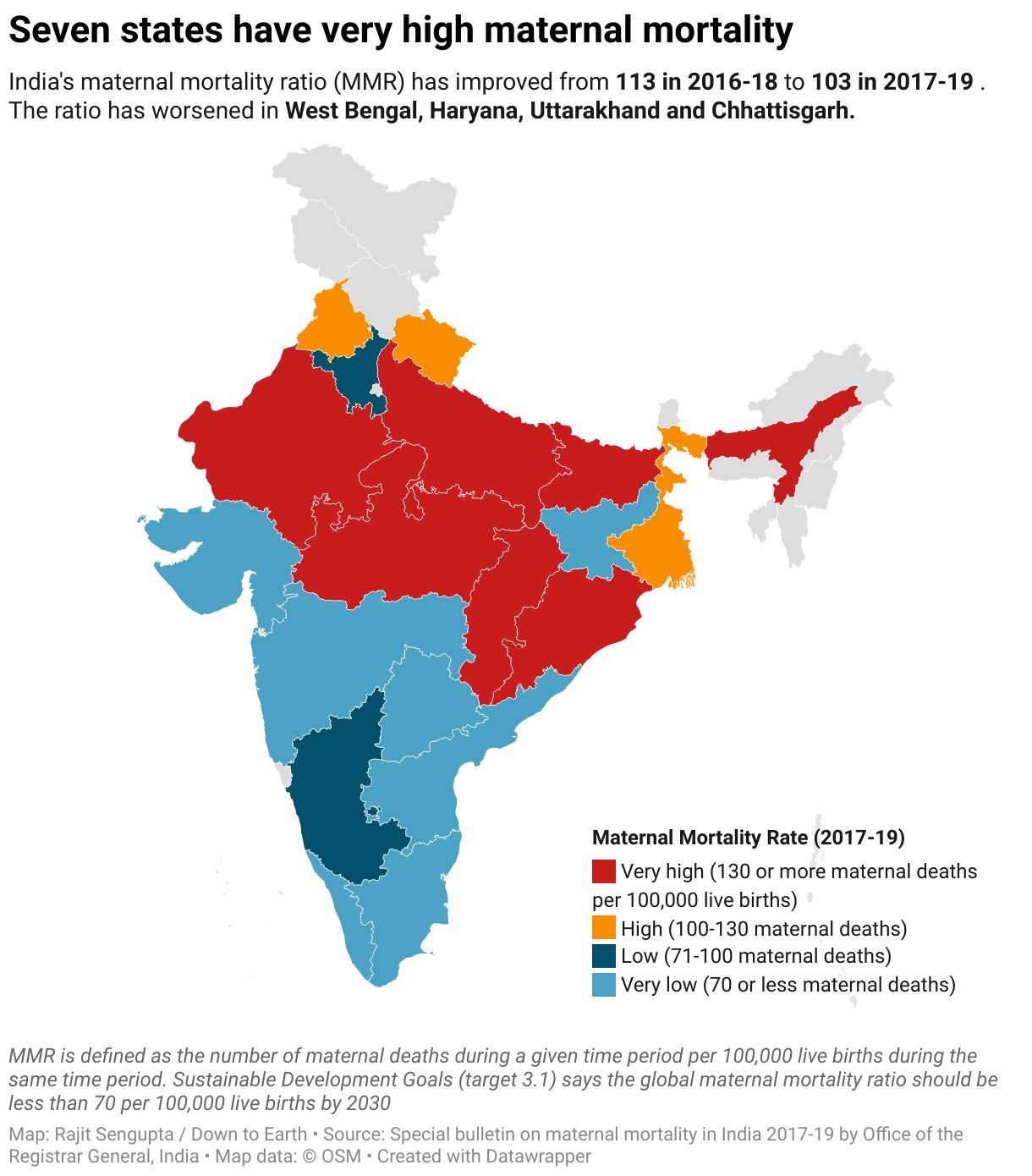
Kerala has yet again emerged on top when it comes to maternal and child health, with the State recording the lowest Maternal Mortality Ratio (MMR) of 30 (per one lakh live births) in the country.
What is Maternal Mortality?
- Maternal mortality refers to deaths due to complications from pregnancy or childbirth.
- The maternal mortality ratio (MMR) is defined as the number of maternal deaths during a given time period per 100,000 live births during the same time period.
- It depicts the risk of maternal death relative to the number of live births and essentially captures the risk of death in a single pregnancy or a single live birth.
Trends in India
- India’s maternal mortality ratio (MMR) has improved to 103 in 2017-19, from 113 in 2016-18.
- Seven Indian states have very high maternal mortality. These are Rajasthan, Uttar Pradesh, Madhya Pradesh, Chhattisgarh, Bihar, Odisha and Assam.
- The MMR is ‘high’ in Punjab, Uttarakhand and West Bengal. This means 100-130 maternal deaths per 100,000 live births.
- It is ‘low’ in Haryana and Karnataka.
- The states of Uttar Pradesh, Rajasthan and Bihar have seen the most drop in MMR.
- West Bengal, Haryana, Uttarakhand and Chhattisgarh have recorded an increase in MMR over the last survey.
Various determinants of maternal health in India

UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Intensified Mission Indradhanush (IMI) 4.0 launched
From UPSC perspective, the following things are important :
Prelims level: Mission Indradhanush
Mains level: Universal vaccination
The Union Health Minister has launched the Intensified Mission Indradhanush (IMI) 4.0.
About IMI 4.0
- The IMI 4.0 will have three rounds and will be conducted in 416 districts (including 75 districts identified for Azadi ka Amrit Mahotsav) across 33 States and UTs, a Health Ministry statement said.
- It will immensely contribute in filling the gaps and make lasting gains towards universal immunisation.
- It will ensure that Routine Immunisation (RI) services reach the unvaccinated and partially vaccinated children and pregnant women” he said.
What is Mission Indradhanush ?
- With the aim to increase the full immunisation coverage, the PM launched Mission Indradhanush in December 2014.
- It aimed to cover the partially and unvaccinated pregnant women and children in pockets of low immunisation coverage, high-risk and hard-to-reach areas and protect them from vaccine preventable diseases.
- The first two phases of the Mission resulted in 6.7% increase in full immunisation coverage in a year.
Aims and objectives
- It aims to immunize all children under the age of 2 years, as well as all pregnant women, against eight vaccine-preventable diseases.
- The diseases being targeted are diphtheria, whooping cough, tetanus, poliomyelitis, tuberculosis, measles, meningitis and Hepatitis B.
- In 2016, four new additions have been made namely Rubella, Japanese Encephalitis, Injectable Polio Vaccine Bivalent and Rotavirus.
- In 2017, Pneumonia was added to the Mission by incorporating the Pneumococcal conjugate vaccine under Universal Immunisation Programme
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Pradhan Mantri Matru Vandana Yojana (PMMVY)
From UPSC perspective, the following things are important :
Prelims level: PMMVY
Mains level: Mother and Child health related schemes
The government’s recent announcement that the maternity benefits program which provides ₹5,000 for the first child will be extended to cover the second child only if it is a girl has met with sharp criticism from activists who have demanded that it be universalized.
What is PMMVY?
- Launched in 2017, this scheme provides ₹5,000 for the birth of the first child to partially compensate a woman for the loss of wages.
- It also aims to improve the nutritional well-being of the mother and the child.
- The amount is given in three installments upon meeting certain conditions.
- It is combined with another scheme, Janani Suraksha Yojana, under which nearly ₹1,000 is given for an institutional birth so that a woman gets a total of ₹6,000.
Eligibility Conditions
The first transfer (at pregnancy trimester) of ₹1,000 requires the mother to:
- Register pregnancy at the Anganwadi Centre (AWC) whenever she comes to know about her conception
- Attend at least one prenatal care session and take Iron-folic acid tablets and TT1 (tetanus toxoid injection)
- Attend at least one counseling session at the AWC or healthcare centre.
The second transfer (six months of conception) of ₹2,000 requires the mother to:
- Attend at least one prenatal care session and TT2
The third transfer (three and a half months after delivery) of ₹2,000 requires the mother to:
- Register the birth
- Immunize the child with OPV and BCG at birth, at six weeks, and at 10 weeks
- Attend at least two growth monitoring sessions within three months of delivery
Additionally, the scheme requires the mother to:
- Exclusively breastfeed for six months and introduce complementary feeding as certified by the mother
- Immunize the child with OPV and DPT
- Attend at least two counselling sessions on growth monitoring and infant and child nutrition and feeding between the third and sixth months after delivery
Why in news?
- Under the revamped PMMVY under Mission Shakti, the maternity benefit amounting to ₹6000 is also to be provided for the second child.
- However, this is only in case the second is a girl child, to discourage pre-birth sex selection and promote the girl child.
Issues with this provision
- To provide maternity benefit only to the mother of the firstborn is illegal as the National Food Security Act, 2013 lays down that every pregnant woman and lactating mother are entitled to it.
- For second child as a girl, it is to promote the birth of a girl child is nothing but posturing since it penalizes the mother for not giving birth to a girl child.
- Subsequent adding of more conditions to the scheme will prove to be a bureaucratic nightmare, which can be overcome if the scheme is universalized.
- Women will be able to access the scheme only after the delivery, which will not have any impact on their nutritional uptake during the course of their pregnancy.
Before judging this factual information, take this PYQ form 2019:
Q.Which of the following statements is/are correct regarding the Maternity Benefit (Amendment) Act, 2017?
- Pregnant women are entitled to three months pre-delivery and three months post-delivery paid leave.
- Enterprises with creches must allow the mother a minimum of six crèche visits daily.
- Women with two children get reduced entitlements.
Select the correct answer using the code given below.
(a) 1 and 2 only
(b) 2 only
(c) 3 only
(d) 1, 2 and 3
Post your answers here.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
HC allows woman to terminate 28-week pregnancy
From UPSC perspective, the following things are important :
Prelims level: Medical Termination of Pregnancy (MTP) Act
Mains level: Reproductive rights of women
The Delhi High Court has permitted a 28-week pregnant woman to undergo medical termination of pregnancy on account of substantial foetal abnormality.
What did the HC rule?
Ans. Termination of Pregnancy is a matter of Right
- The High Court said the woman cannot be deprived of the freedom to take a decision to continue or not to continue with the pregnancy, due to foetal abnormalities.
- HC ruled that reproductive choice is a dimension of personal liberty that is enshrined in Article 21 of the Constitution.
- It stated that allowing the pregnancy to continue would have a deleterious impact on the petitioner’s mental health.
- The petitioner cannot be deprived of the freedom to take a decision to continue or not to continue with the pregnancy in view the medical board’s opinion.
What is the Medical Termination of Pregnancy (MTP) Act?
- Abortion in India has been legal under various circumstances for the last 50 years with the introduction of MTP Act in 1971.
- The Act was amended in 2003 to enable women’s accessibility to safe and legal abortion services.
Termination of pregnancy is permitted for a broad range of conditions up to 20 weeks of gestation as detailed below:
- Threat to mother: When the continuation of pregnancy is a risk to the life of a pregnant woman or could cause grave injury to her physical or mental health;
- Child abnormalities: When there is substantial risk that the child, if born or dead would be seriously handicapped due to physical or mental abnormalities;
- Rape survivors: When pregnancy is caused due to rape (presumed to cause grave injury to the mental health of the woman);
- Failure of contraception: When pregnancy is caused due to failure of contraceptives used by a married woman or her husband (presumed to constitute grave injury to mental health of the woman).
Conditions for abortion
- The MTP Act specifies – (i) who can terminate a pregnancy; (ii) till when a pregnancy can be terminated; and (iii) where can a pregnancy be terminated.
- There must be an opinion formed of a doctor, that the pregnancy would cause a risk to the life of the pregnant woman or grave injury to her physical or mental health.
- When a pregnancy exceeds 20 weeks but not 24 weeks, termination is permissible on the opinion formed of two registered medical practitioners.
What was the recent case?
- In the present case, the woman has completed 28 weeks of pregnancy.
- As the MTP Act does not permit pregnancy termination beyond 24 weeks, she approached the court.
- Various anomalies were found in the heart of the foetus in the foetal ECG.
Key issues
There are differing opinions with regard to allowing abortions.
- One opinion is that terminating a pregnancy is the choice of the pregnant woman and a part of her reproductive rights.
- The other is that the state has an obligation to protect life, and hence should provide for the protection of the foetus.
- Across the world, countries set varying conditions and time limits for allowing abortions, based on foetal health, and risk to the pregnant woman.
Conclusion
- Access to abortion facilities is limited not just by legislative barriers but also the fear of judgment from medical practitioners.
- It is imperative that healthcare providers be sensitized towards being scientific, objective and compassionate in their approach to abortions.
Also read
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Risks of mandatory Iron Fortification
From UPSC perspective, the following things are important :
Prelims level: Iron fortification
Mains level: Isuses with fortified food
Many things have been said about the necessity for mandatory iron fortification of foods in India.
Iron fortification
- Iron fortification of food is a methodology utilized worldwide to address iron deficiency.
- A critical problem in some food fortification programs is the lack of bioavailability of iron compounds.
Why need iron fortification?
Ans. Prevalence of Anaemia
- Iron deficiency anaemia is due to insufficient iron.
- National Family Health Survey (NFHS)-5 provides insights into anaemia prevalence in the country, indicating that 57.2% of women ages 15 to 49 are anaemic, up from 49.7% in NFHS-4.
- Without enough iron, the body can’t produce enough of a substance in red blood cells that enables them to carry oxygen (hemoglobin).
- Severe anemia during pregnancy increases your risk of premature birth, having a low birth weight baby and postpartum depression.
- Some studies also show an increased risk of infant death immediately before or after birth.
Concerns over iron fortification
Ans. Fear of diabetes and heart ailments
- Iron increases the risk for many non-communicable diseases like diabetes, hypertension and even high blood cholesterol.
- A US based survey shows that high ferritin level had a four-fold higher risk of having diabetes.
- The Comprehensive National Nutrition Survey of Indian adolescents to resulted in such scary outcomes.
- There was a clear and significant risk for each of these conditions as serum ferritin increased.
India’s vulnerability
Ans. India is world capital of diabetes and hypertension
- No less than 50% of Indian children, aged 5-19 years, already had a biomarker of either high blood sugar or high blood lipids, even when thin or stunted.
- Thus, the risk of chronic disease is already very high in our children.
- Thus mandatory cereal fortification has severe hazards for India.
Why mandatory fortification is not a feasible option?
- Occurrence of deficiencies: We do not even know if anaemia is as rampant to warrant such mandatory measures.
- Manipulating food choices: When mandatory fortification is enforced in parts of the population that do not need this, it removes their choice of foods, or autonomy.
- Morbidities due to excess: It could even be unethical if the risk of other morbidities is increased.
- No successful example: Rice fortification has not been shown to work in a combined analysis.
Conclusion
- Food fortification is not a magic bullet.
- It should be viewed as a complementary strategy for the prevention and control of micronutrient deficiencies.
- As dietary patterns and deficiency states change, monitoring and periodic evaluation will be essential in helping to make necessary changes.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Project Sampoorna: A successful measure against malnutrition
From UPSC perspective, the following things are important :
Prelims level: Project Sampoorna
Mains level: Innovative measures against malnutrition
Project Sampoorna’s success in reducing child malnutrition is a model that can be easily implemented anywhere.
What is Project Sampoorna?
- Project Sampoorna has been implemented in the Bongaigaon district of Assam.
- It aims to target Severe Acute Malnutrition (SAM) and Moderate Acute Malnutrition (MAM).
- It was launched to target the mothers of SAM/ MAM children with the tagline being ‘Empowered Mothers, Healthy Children’.
- It was based on the success of the community-based COVID-19 management model (Project Mili Juli).
Key features of the project
- Under this project, the mother of a healthy child of an Anganwadi Centre was paired with the target mother and they would be Buddy Mothers.
- They were usually neighbours and shared similar socioeconomic backgrounds.
- They were given diet charts to indicate the daily food intake of their children and would have discussions on all Tuesdays at the Anganwadi centres.
- 100 millilitres of milk and an egg on alternate days for the children for the first 3 months were provided so that their mothers could stabilise themselves in the newly found jobs.
- Children who had not improved were checked and treated by doctors under the Rashtriya Bal Swasthya Karyakram (RBSK).
Success of the project
- This project has prevented at least 1,200 children from becoming malnourished over the last year.
- National Nutrition Mission and the State government recognised this project in the ‘Innovation Category’.
- The mothers were enrolled in Self Help Groups (SHGs) under the National Rural Livelihoods Mission (NRLM) and were thus working.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Nationwide Pneumococcal Conjugate Vaccine (PCV) drive launched
From UPSC perspective, the following things are important :
Prelims level: PCV
Mains level: Not Much
Union Health Minister has launched a nationwide expansion of Pneumococcal 13-valent Conjugate Vaccine (PCV) under the Universal Immunisation Programme (UIP).
Why such drive?
- Pneumonia was a leading cause of death among children under five, globally and in India.
- Pneumonia caused by pneumococcus is the most common cause of severe pneumonia in children.
- Around 16% of deaths in children occur due to pneumonia in India.
- The nationwide roll-out of PCV will reduce child mortality by around 60%.
Pneumococcal Conjugate Vaccine (PCV)
- The PCV is a mix of several bacteria of the pneumococci family, which are known to cause pneumonia—hence ‘conjugate’ is included in the name of the vaccine.
- PCV prevents pneumococcal disease. It can protect both children and adults from pneumococcal disease.
- Such conjugate vaccines are made using a combination of two different components.
Pneumonia vs Pneumococcal pneumonia
- Pneumonia is a lung disease.
- Pneumococcal pneumonia, a kind of pneumonia, can infect the upper respiratory tract and can spread to the blood, lungs, middle ear, or nervous system.
- Pneumococcal disease is a name for any infection caused by bacteria called Streptococcus pneumonia or pneumococcus.
- Most people carry pneumococcus in their nose and throat, where the bacteria do not cause any symptoms.
Take this yorker from CSP 2020:
Q.What is the importance of using Pneumococcal Conjugate Vaccines in India?
- These vaccines are effective against pneumonia as well as meningitis and sepsis.
- Dependence on antibiotics that are not effective against drug-resistant bacteria can be reduced.
- These vaccines have no side effects and cause no allergic reactions.
Select the correct answer using the code given below:
(a) 1 only
(b) 1 and 2 only
(c) 3 only
(d) 1, 2 and 3
Post your answers here.
UPSC 2022 countdown has begun! Get your personal guidance plan now! (Click here)
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Jharkhand’s SAAMAR campaign to fight malnutrition
From UPSC perspective, the following things are important :
Prelims level: SAAMAR campaign
Mains level: Various facets of hunger and malnutrition in India
The Jharkhand government has announced the launch of the SAAMAR campaign to tackle malnutrition in the state.
We can expect an MCQ like:
Q.SAAMAR campaign sometimes seen in news is related to:
() Bovine health
() Mother and Child Health
() Non-communicable diseases
() None of these
SAAMAR
- SAAMAR is an acronym for Strategic Action for Alleviation of Malnutrition and Anemia Reduction.
- The campaign aims to identify anaemic women and malnourished children and converge various departments to effectively deal with the problem in a state where malnutrition has been a major problem.
- Every second child in the state is stunted and underweight and every third child is affected by stunting and every 10th child is affected by severe wasting and around 70% of children are anaemic NFHS-4 data.
Features of the scheme
- Although existing schemes are there, seeing the current situation, the intervention was required with a ‘different approach to reduce malnutrition.
- SAAMAR has been launched with a 1000 days target, under which annual surveys will be conducted to track the progress.
- It talks of convergence of various departments such as the Rural Development Department and Food and Civil Supplies and engagement with school management committees, gram sabhas among others and making them aware of nutritional behaviour.
- Most importantly, the campaign, as per the note, also tries to target Primarily Vulnerable Tribal Groups.
Outlined strategy under the scheme
- To tackle severe acute malnutrition children, every Anganwadi Centres will be engaged to identify these children and subsequently will be treated at the Malnutrition Treatment Centres.
- In the same process, the anaemic women will also be listed and will be referred to health centres in serious cases.
- All of these will be done by measuring Mid-Upper Arm Circumference (MUAC) of women and children through MUAC tapes and Edema levels.
- Angawadi’s Sahayia and Sevika will take them to the nearest Health Centre where they will be checked again and then registered on the portal of State Nutrition Mission.
Why need such a scheme?
- The state government runs various schemes under Child Development Schemes, National Nutrition Mission among others to deal with the situation, but it is not enough.
- Dealing with malnutrition in the state monitoring has been an important concern due to the lack of doctors or health care workers.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Rajya Sabha passes MTP Bill, 2020
From UPSC perspective, the following things are important :
Prelims level: MTP Act
Mains level: Termination of Pregnancy (MTP) and associated issues
The Rajya Sabha has passed the Medical Termination of Pregnancy (Amendment) Bill, 2020 that increases the time period within which an abortion may be carried out.
What are the differing opinions with regards to the Termination of Pregnancy (MTP) Amendment Bill, 2020? Discuss.
MTP Bill, 2020
The MTP Bill was passed in Lok Sabha in March 2020. Its salient features included:
- Proposing requirement for the opinion of one provider for termination of pregnancy, up to 20 weeks of gestation and introducing the requirement of the opinion of two providers for termination of pregnancy of 20-24 weeks of gestation.
- Enhancing the upper gestation limit from 20 to 24 weeks for special categories of women which will be defined in the amendments to the MTP Rules and would include ‘vulnerable women including survivors of rape, victims of incest and other vulnerable women (like differently-abled women, Minors) etc.
- Upper gestation limit not to apply in cases of substantial foetal abnormalities diagnosed by Medical Board. The composition, functions and other details of the Medical Board to be prescribed subsequently in Rules under the Act.
- Anonymity of the person: The name and other particulars of a woman whose pregnancy has been terminated shall not be revealed except to a person authorised in any law for the time being in force.
Benefits sought with the bill
- It is seen as a step towards the safety and well-being of the women and many women will be benefitted from this.
- Recently several petitions were received by the Courts seeking permission for aborting pregnancies at a gestational age beyond the present permissible limit on grounds of foetal abnormalities or pregnancies due to sexual violence faced by women.
- The proposed increase in gestational age will ensure dignity, autonomy, confidentiality and justice for women who need to terminate the pregnancy.
Flaws in the bill
- The Bill allows abortion after 24 weeks only in cases where a Medical Board diagnoses substantial foetal abnormalities.
- This implies that for a case requiring abortion due to rape, that exceeds 24-weeks, the only recourse remains through a Writ Petition.
- The Bill does not specify the categories of women who may terminate pregnancies between 20-24 weeks and leaves it to be prescribed through Rules.
- The Act (and the Bill) requires an abortion to be performed only by doctors with a specialization in gynaecology or obstetrics.
- As there is a 75% shortage of such doctors in community health centres in rural areas, pregnant women may continue to find it difficult to access facilities for safe abortions.
Key Issues and Analysis
- There are differing opinions with regard to allowing abortions. One opinion is that terminating a pregnancy is the choice of the pregnant woman and a part of her reproductive rights.
- The other is that the state has an obligation to protect life, and hence should provide for the protection of the foetus.
- Across the world, countries set varying conditions and time limits for allowing abortions, based on foetal health, and risk to the pregnant woman.
- Several Writ Petitions have been filed by women seeking permission to abort pregnancies beyond 20-weeks due to foetal abnormalities or rape.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Intensified Mission Indradhanush (IMI) 3.0
From UPSC perspective, the following things are important :
Prelims level: Mission Indradhanush
Mains level: Universal immunization programme
States and UTs have started the implementation of the Intensified Mission Indradhanush 3.0, a campaign aimed to reach those children and pregnant women who have been missed out or been left out of the routine immunisation.
Do not get confused with the Mission Indradhanush for Public Sector Banks launched in 2015. It aims at revamping the functioning of the Public Sector Banks to enable them to compete with the Private Sector Banks.
Intensified Mission Indradhanush (IMI) 3.0
- IMI 3.0 is aimed to accelerate the full immunization of children and pregnant women through a mission mode intervention.
- The campaign is scheduled to have two rounds of immunisation lasting 15 days (excluding routine immunisation and holidays).
- It is being conducted in pre-identified 250 districts/urban areas across 29 States/UTs in the country.
- Beneficiaries from migration areas and hard to reach areas will be targeted as they may have missed their vaccine doses during the pandemic.
About the Mission Indradhanush
- Mission Indradhanush seeks to drive towards 90% full immunisation coverage of India and sustain the same by the year 2020. It was launched in December 2014.
Aims and objectives
- It aims to immunize all children under the age of 2 years, as well as all pregnant women, against eight vaccine-preventable diseases.
- The diseases being targeted are diphtheria, whooping cough, tetanus, poliomyelitis, tuberculosis, measles, meningitis and Hepatitis B.
- In 2016, four new additions have been made namely Rubella, Japanese Encephalitis, Injectable Polio Vaccine Bivalent and Rotavirus.
- In 2017, Pneumonia was added to the Mission by incorporating the Pneumococcal conjugate vaccine under Universal Immunisation Programme
Try this question from CSP 2016:
Q.‘Mission Indradhanush’ launched by the Government of India pertains to:
(a) Immunization of children and pregnant women
(b) Construction of smart cities across the country
(c) India’s own search for the Earth-like planets in outer space
(d) New Educational Policy
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[pib] National Creche Scheme
From UPSC perspective, the following things are important :
Prelims level: Creche scheme
Mains level: Maternity benefits act

The Union Minister of Women and Child Development have given information about the National Creche Scheme to the Lok Sabha.
Try this PYQ:
Q.Which of the following statements is/are correct regarding the Maternity Benefit (Amendment) Act, 2017?
- Pregnant women are entitled to three months pre-delivery and three months post-delivery paid leave.
- Enterprises with creches must allow the mother a minimum of six crèche visits daily.
- Women with two children get reduced entitlements.
Select the correct answer using the code given below.
(a) 1 and 2 only
(b) 2 only
(c) 3 only
(d) 1, 2 and 3
National Creche Scheme
- The Ministry of WCD implements the NCS for the children of working mothers as a Centrally Sponsored Scheme through States/ UTs with effect from 01.01.2017.
- It aims to provide daycare facilities to children (age group of 6 months to 6 years) of working mothers.
The Scheme provides an integrated package of the following services:
- Daycare facilities including sleeping facilities.
- Early stimulation for children below 3 years and pre-school education for 3 to 6 years old children
- Supplementary nutrition (to be locally sourced)
- Growth monitoring
- Health check-up and immunization
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
MTP amendment Bill
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2- MTP (Amendment) Bill and issues with it
The article discusses the provision of the medical board in the MTP (Amendment) Act and issues with it.
Proposal of medical board
- The Medical Termination of Pregnancy (Amendment) Bill (‘MTP Bill’) passed in the Lok Sabha is scheduled to be tabled for consideration in Rajya Sabha.
- The Act prescribes the setting up of medical boards in every state and Union territory (UT), consisting of a gynaecologist, paediatrician, radiologist or sonologist and any other members as proposed by that state or UT.
- Each board will be responsible for diagnosing substantial foetal abnormalities that necessitate termination of pregnancy after a 24-week gestation period.
- Medical boards are a form of third-party authorisation and were not envisaged in the MTP Act, 1971.
Issues with the proposal
- In the context of the current healthcare budgetary challenges, this proposal to set up infrastructure across the country to regulate medical termination of pregnancies is both financially unsound and practically impossible.
- India’s healthcare system has neither the financial investment nor the infrastructure to sustain the operation and functioning of medical boards in every state and UT.
- Due to the weak healthcare infrastructure in the country, it would be practically impossible to constitute these boards with the requisite specialists.
- Even where they are set up, the accessibility of such boards for pregnant persons, especially those living in rural areas, remains a major challenge.
- More importantly, subjecting people to multiple invasive examinations is a grave violation of their rights to privacy and dignity.
- Requiring pregnant persons to navigate a bureaucratic web of authorisation will inevitably lead to delays and thereby impede access to safe and legal abortion services.
Poor public financing and privatisation of healthcare
- At 1.6 per cent of GDP in 2019-20 India’s current level of public financing of health is one of the lowest in the world
- This has meant that most health expenditure in the country is out of pocket (OOP) — borne by patients themselves.
- OOP expenditure on healthcare is recorded at 58.7 per cent as per the National Health Accounts in 2016-17.
- The central government has preferred to incentivise private players to set up or offer services, instead of building infrastructural and professional capacity.
- Privatisation drives up costs of care and the handing over of public facilities to the private sector can have catastrophic consequences.
- They additionally remain non-accountable to state authorities in terms of affordability or transparency for instance, through Right to Information enquiries, or to uphold fundamental rights like non-discrimination in treatment or employment, or even the fundamental right to health.
- The National Sample Survey Organisation (NSSO)’s 75th report shows that less than 20 per cent of the population is covered by health insurance in India.
- According to the National Health Profile 2017, India has only one doctor for roughly 10,200 people in the public sector.
Consider the question “Discsss the changes made by the Medical Termination of Pregnancy (Amendment) Bill and the challenges its provision could face.”
Conclusion
Poor public health infrastructure and absence of specialists across the country have meant that most abortions do not happen in the public sector, but at private centres or at home. With overwhelming shortfalls in specialist availability, especially in rural and scheduled areas, it would be impossible to constitute boards with requisite specialist representation as contemplated under the MTP Bill.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Pradhan Mantri Matru Vandana Yojana (PMMVY)
From UPSC perspective, the following things are important :
Prelims level: PMMVY
Mains level: Maternity healthcare
The government’s maternity benefit scheme, or Pradhan Mantri Matru Vandana Yojana, has crossed 1.75 crores, eligible women, till the financial year 2020, the Centre informed Parliament.
PMMVY
- The PMMVY is a maternity benefit program introduced in 2017 and is implemented by the Ministry of Women and Child Development.
- It is a conditional cash transfer scheme for pregnant and lactating women of 19 years of age or above for the first live birth.
- It provides partial wage compensation to women for wage-loss during childbirth and childcare and to provide conditions for safe delivery and good nutrition and feeding practices.
- Under the scheme, pregnant women and lactating mothers receive ₹5,000 on the birth of their first child in three instalments, after fulfilling certain conditionalities.
- In 2013, the scheme was brought under the National Food Security Act, 2013 to implement the provision of cash maternity benefit stated in the Act.
- The direct benefit cash transfer is to help expectant mothers meet enhanced nutritional requirements as well as to partially compensate them for wage loss during their pregnancy.
Eligibility Conditions and Conditionalities
The first transfer (at pregnancy trimester) of ₹1,000 requires the mother to:
- Register pregnancy at the Anganwadi Centre (AWC) whenever she comes to know about her conception
- Attend at least one prenatal care session and taking Iron-folic acid tablets and TT1 (tetanus toxoid injection), and
- Attend at least one counselling session at the AWC or healthcare centre.
The second transfer (six months of conception) of ₹2,000 requires the mother to:
- Attend at least one prenatal care session and TT2
The third transfer (three and a half months after delivery) of ₹2,000 requires the mother to:
- Register the birth
- Immunize the child with OPV and BCG at birth, at six weeks and at 10 weeks
- Attend at least two growth monitoring sessions within three months of delivery
Additionally, the scheme requires the mother to:
- Exclusively breastfeed for six months and introduce complementary feeding as certified by the mother
- Immunize the child with OPV and DPT
- Attend at least two counselling sessions on growth monitoring and infant and child nutrition and feeding between the third and sixth months after delivery
Before judging this factual information, take this PYQ form 2019:
Q.Which of the following statements is/are correct regarding the Maternity Benefit (Amendment) Act, 2017?
- Pregnant women are entitled to three months pre-delivery and three months post-delivery paid leave.
- Enterprises with creches must allow the mother a minimum of six crèche visits daily.
- Women with two children get reduced entitlements.
Select the correct answer using the code given below.
(a) 1 and 2 only
(b) 2 only
(c) 3 only
(d) 1, 2 and 3
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Paternity Leave in India
From UPSC perspective, the following things are important :
Prelims level: Not Much
Mains level: Parental care and associated societal perspectives

Indian cricket captain has opted for paternity leave amidst an ongoing tournament. This has led to his criticism as well as praise for prioritizing family.
Q.Paternity leave is one of the solutions which can help in ending the “motherhood penalty”. Examine with context to working mothers.
What is Paternity leave?
- Paternity leave is a short period of leave for the father to take immediately following childbirth to help care for the child and assist the mother.
- Parental leave is a longer period of leave granted to look after the infant child, usually after the expiration of paternity/maternity leave.
Legal Aspects of Paternity Leave in India
There is no specific or explicit law for paternity leave in India.
- Maternity leave is governed by the Maternity Benefit Act, 1961 which was last amended in 2017 to enhance the period of maternity leave to 26 weeks from the previous 12 weeks.
- The Central Civil Service (Leave Rules), 1972 allows for 15 days of paid paternity leave before childbirth or up to 6 months from the date of the delivery of the child.
- An attempt was made to introduce a pan India legislation on paternity leave in 2017 as a private member’s bill in Lok Sabha, but it was not successful.
- The Paternity Benefit Bill, 2017, provided for a paid leave of fifteen days which could be availed up to three months from the date when the child was born.
- It also included an adopted child below the age of three months and applied to men in the organised i.e. private as well as unorganised sectors.
Popular trends
- The longest leave –– six months –– is provided by Ikea, which extends rules from home country Sweden to India.
- Among Indian companies, Zomato made news in 2019 when it decided to give 26-week paternity leave to its employees.
Precursors in India
- The Central Government recently announced that male government employees who are ‘single parents’ which included widowers, divorcees, or unmarried men raising children single-handedly would now be entitled to “child care leave” (CCL).
- Here, they would receive 100% of the leave salary for the first 365 days of leave and 80% of leave salary for the next 365 days.
- This leave was previously only available to women employees.
Why paternity leave matters?
- Most working new mothers (for those who can make that choice) opt for maternity leave either just before the birth or after childbirth.
- It paves the way for at least their temporary, and sometimes their permanent exit from the workplace.
- On the other hand, not many fathers experience much difference in their employment and workplace situation after their child is born, which may either be voluntary by not taking time off or involuntary.
- This structural difference is one of the key components that influence gender dynamics both in the workplace and at home.
The gender dynamics behind
- Lack of paternity leave not only robs new fathers of the crucial chance to bond with their newborn child but also reinforces women’s role as the primary caregiver and underpins the belief that child care is predominantly the mother’s job.
- Paternity leave is a way to directly address the gender dynamic that prevails both at the workplace and at home.
- The undue burden of childcare that is placed on women at home is bound to and does, spill over into their workplace and professional lives.
- The natural effect of it is that it puts hurdles across women’s careers and might slow their growth prospects while some women might choose to quit altogether.
Way forward
- By only having maternity leaves and not giving due consideration to paternity leave, the stereotype that women belong at home, taking care of children is reinforced.
- By no means is the introduction of paternity leave a panacea for gendered workplaces, but it will be a significant step in combating and overcoming stereotype.
- For India, a decent way to begin would be to have a national policy on paternity leave that would include all fathers and would apply irrespective of whether they worked in the organised or unorganised sectors.
- Shifting from a purely maternity oriented care framework to a parental care framework which would involve both parents would be beneficial for all stakeholders and is what we need today.
Conclusion
- A major benefit that accrues from paternity leave is that it eases pressure and stigma from women at the workplace, as they no longer are the only ones who are taking leave for child care purposes.
- Paternity leave is also one of the solutions which can help in ending the “motherhood penalty”.
- The motherhood penalty is a term that describes the disadvantages that women with children face as compared to women who don’t in workplaces.
- Fathers need to be active co-parents and not just helpers to their female partners/wives.
- And for ones with feminist’s perspectives, they should not look paternity leave as a sole vacation for men.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Improving the diet of low income households to address malnutrition
From UPSC perspective, the following things are important :
Prelims level: National Family Health Survey
Mains level: Paper 2- Problems of malnutrition and issues with it
The article suggests the ways to deal with the menace of malnutrition in the country.
Findings of the first phase of NFHS-5
- Recently, the first phase of the NFHS-5 survey was published.
- The deteriorating nutrition and anaemia indicators, especially among children is a cause for concern.
- More deterioration in nutrition indicators following the COVID-19 pandemic is feared in the next phase of NFHS-5.
- This deterioration would be on account of loss of livelihoods, reduced food consumption among the poor and disruption of government nutrition programmes.
Challenges
- Unlike a disease outbreak there may not be any popular demand to address malnutrition — the public, by and large, does not have adequate information about the damage malnutrition causes.
- Hence, in the Indian context, it becomes the responsibility of the government/civil society to first provide information and awareness to the community about malnutrition.
Steps to be taken
- The government should examine the current nutrition-related programmes, and analysing why they are not able to reduce malnutrition faster.
- Additional interventions could be introduced in pockets, identified as high-burden districts.
- There should be different norms and more intensive interventions within the ICDS for these chronically malnourished pockets.
- We need to know if the National Nutrition Policy 1993 is still operational.
- If not, it seems that we are attempting to address this problem without a policy framework or plan of action.
Addressing the root cause of malnutrition in India
The following three deficits are the root cause of malnutrition in India.
1) Dietary deficit
- There is a large dietary deficit among at least 40 per cent of our population of all age groups, shown in— the National Nutrition Monitoring Bureau’s Third Repeat Survey (2012), NFHS 4, 2015-16, the NNMB Technical Report Number 27, 2017.
- Our current interventions are not being able to bridge this protein-calorie-micronutrient deficit.
- The NHHS-4 and NFHS-5 surveys reveal an acute dietary deficit among infants below two years, and considerable stunting and wasting of infants below six months.
- Unless this maternal/infant dietary deficit is addressed, we will not see rapid improvement in our nutritional indicators.
2) Information deficit at household level
- We do not have a national IEC (information, education and communication) programme that reaches targeted households to bring about the required behavioural change regarding some basic but critical facts.
- For example, IEC tells about the importance of balanced diets in low-income household budgets, proper maternal, child and adolescent nutrition and healthcare.
3) Inequitable market conditions
- The largest deficit, which is a major cause of dietary deficiency and India’s chronic malnutrition, pertains to inequitable market conditions.
- Such market conditions deny affordable and energy-fortified food to children, adolescents and adults in lower-income families.
- The market has stacks of expensive fortified energy food and beverages for higher income groups, but nothing affordable for low-income groups.
Conclusion
Raising the diet of our people from subsistence level to higher levels of nourishment by overcoming the triple deficit is the only way to improve the nutritional indicators of our population — amongst children, adolescents and adults.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Need to focus on the well-being of the child from womb to first five years
From UPSC perspective, the following things are important :
Prelims level: Trends in the various data of NFHS
Mains level: Paper 2- Analysis of NFHS-5 data
The article analyses the data of NHFS-5 and try to factors responsible for the outcomes.
Analysing health and nutrition of child through NHFS-5
- The recently released fifth round of the National Family Health Survey (NFHS-5) provide insights into some dimensions of micro-development performance before COVID struck.
- The latest round only has data for 17 states and five Union territories.
- Madhya Pradesh, Uttar Pradesh, Punjab, Rajasthan and Tamil Nadu are notable exclusions.
- Many of the child-related outcomes are also determined by state-level implementation, therefore neither success nor failure can be attributed to state or the centre alone.
Let’s understand the data
- The NFHS has 42 indicators related to child’s health and nutrition.
- Indicators fall into nine categories and each of these can be divided into outcomes and inputs.
- For example, neonatal, infant and under-5 mortality rates can be thought of as outcomes.
- Similarly, all the nutrition indicators —stunting, wastage, excess wastage, underweight and overweight can also be classified as outcomes.
- In contrast, the post-natal care indicators relating to visits made by health workers and the extent and nature of feeding for the child can be classified as inputs.
Outcomes of the survey
- On the front of wasting (weight for height of children) these is an improvement because even though the gains were marginal, they reversed a negative trend between 2005 and 2015.
- India continues to be successful in preventing child deaths, but the health and nutrition of the surviving, living child has deteriorated, somewhat worryingly.
- India continued to make progress in preventing child-related deaths (neonatal, infants and under-5).
- The pace of improvement in child mortality slowed down relative to the previous 10 years (Fig.1).
- Figure 2 shows the six indicators where outcomes have deteriorated. These all relate to what happens after survival:
- The health (anaemia, diarrhoea, and acute respiratory illness (ARI)) and nutrition (stunting, and overweight) of the child deteriorated between 2015 and 2019.
- The absolute deterioration in health and nutrition indicators must be seen against the fact that they reversed the historic trends of steady improvements.
What explains the outcomes
- Implementation capacity of individual states probably played an important role.
- Sector-specific factors such as changing diets are also implicated.
- A broader deterioration in outcomes hints at the likelihood of a common factor, namely the macro-economic growth environment, which determines employment, incomes and opportunities.
- At the least, it is safe to conjecture that some of these outcomes are inconsistent with the narrative of a rapidly growing economy.
Conclusion
As discussed in Chapter 5 of the Economic Survey of 2015-16, perhaps the next big welfare initiative of the government should be a mission-mode focus on the well-being of the early child (and of course the mother), from the womb to the first five years, which research shows is critical for realising its long run potential as an individual.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Burden of Anaemia in India
From UPSC perspective, the following things are important :
Prelims level: Anaemia
Mains level: Anaemia
Indian women and children are overwhelmingly anaemic, according to the National Family Health Survey (NFHS) 2019-20 released this month, and the condition is the most prevalent in the Himalayan cold desert.
Anaemia is the condition of having a lower-than-normal number of red blood cells or a quantity of haemoglobin. How widespread is it in India?
What is Anaemia?
- The condition of having a lower-than-normal number of red blood cells or a quantity of haemoglobin. It can make one feel tired, cold, dizzy, and irritable, and short of breath, among other symptoms.
- A diet that does not contain enough iron, folic acid, or vitamin B12 is a common cause of anaemia.
- Some other conditions that may lead to anaemia include pregnancy, heavy periods, blood disorders or cancer, inherited disorders, and infectious diseases.
How widespread is anaemia in our country?
- In Phase I of the NHFS, result factsheets have been released for 22 states and UTs.
- In a majority of these states and UTs, more than half the children and women were found to be anaemic.
- In 15 of these 22 states and UTs, more than half the children are anaemic. Similarly, more than 50 percent of women are anaemic in 14 of these states and UTs.
- The proportion of anaemic children and women is comparatively lower in Lakshadweep, Kerala, Meghalaya, Manipur, Mizoram, and Nagaland.
- However, it is higher in Ladakh, Gujarat, J&K, and West Bengal, among others.
- Anaemia among men was less than 30 percent in a majority of these states and UTs.
What was the methodology used?
- NFHS used the capillary blood of the respondents for the estimation of anaemia. For children, haemoglobin of fewer than 11 grams per decilitre (g/dl) indicated anaemia.
- For non-pregnant and pregnant women, it was less than 12 g/dl and 11g/dl respectively, and for men, it was less than 13 g/dl.
- Among children, the prevalence was adjusted for altitude and among adults, it was adjusted for altitude and smoking status.
Why is anaemia so high in the country?
- Iron-deficiency and vitamin B12-deficiency anaemia are the two common types of anaemia in India.
- Among women, iron deficiency prevalence is higher than men due to menstrual iron losses and the high iron demands of a growing foetus during pregnancies.
- Lack of millets in the diet due to overdependence on rice and wheat, insufficient consumption of green and leafy vegetables could be the reasons behind the high prevalence of anaemia in India.
What about the cold desert region of the western Himalaya?
- In the union territory of Ladakh, a whopping 92.5 per cent children, 92.8 per cent women, and around 76 per cent men are anaemic in the given age groups, as per the survey.
- The high prevalence in this region could be due to the short supply of fresh vegetables and fruits during the long winter each year.
- Crops here are generally only grown in summer and during winter; residents fail to get a regular supply of green vegetables and fresh produce from outside, due to restricted connectivity in harsh weather.
- However, there could be other factors as well and the causes of anaemia here are yet to be scientifically ascertained.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
India needs to rethink its nutrition agenda
From UPSC perspective, the following things are important :
Prelims level: NFHS
Mains level: Various facets of hunger and malnutrition in India
Poor nutritional outcomes in NFHS-5 show that a piecemeal approach does not work.
Nutrition-related data released by NFHS-5
- The Ministry of Health and Family Welfare has released data fact sheets for 22 States and Union Territories (UTs) based on the findings of Phase I of the National Family Health Survey-5 (NFHS-5).
- The 22 States/ UTs don’t include some major States such as Tamil Nadu, Rajasthan, Punjab, Uttar Pradesh, Jharkhand, Odisha and Madhya Pradesh.
Practice Question: The latest findings from the National Family Health Survey data shows a sign of worry. Suggest the policy measures required to tackle the health and nutrition-related issues in India.
Worrying findings
- There is an increase in the prevalence of severe acute malnutrition in 16 States/UTs (compared to NFHS-4 conducted in 2015-16). Kerala and Karnataka are the only two big states where there is some decline.
- The percentage of children under five who are underweight has also increased in 16 out of the 22 States/UTs.
- Anaemia levels among children as well as adult women have increased in most of the States with a decline in anaemia among children being seen only in four States/UTs.
- There is also an increase in the prevalence of other indicators such as adult malnutrition in many States/ UTs.
- Most States/UTs also see an increase in overweight/obesity prevalence among children and adults shows the inadequacy of diets in India both in terms of quality and quantity.
- The data report an increase in childhood stunting (an indicator of chronic under-nutrition and considered a sensitive indicator of overall well-being) in 13 of the 22 States/UTs.
- Poshan Abhiyaan, one of the flagship programmes of the PM, launched in 2017, aimed at achieving a 2% reduction in childhood stunting per year.
Economic growth vs health indicators
- There is an increase in the prevalence of childhood stunting in the country during the period 2015-16 to 2019-20.
- This calls for serious introspection on not just the direct programmes in place to address the problem of child malnutrition but also the overall model of economic growth that the country has embarked upon.
- The World Health Organization calls stunting “a marker of inequalities in human development”.
- Over the last three decades, India has experienced high rates of economic growth. But this period has also seen increasing inequality, greater informalisation of the labour force, and reducing employment elasticities of growth.
- Currently, India is witnessing a slowdown in economic growth, stagnant rural wages and highest levels of unemployment. This is reflected in the rising number of reported starvation deaths from different parts of the country.
- The situation has become even worse due to the pandemic and lockdown-induced economic distress.
- Field surveys such as the recent ‘Hunger Watch’ are already showing massive levels of food insecurity and decline in food consumption, especially among the poor and vulnerable households.
- All of this calls for urgent action with commitment towards addressing the issue of malnutrition.
Social protection schemes and their impact on nutrition indicators
- Social protection schemes and public programmes such as the Mahatma Gandhi National Rural Employment Guarantee Scheme, the Public Distribution System, the Integrated Child Development Scheme (ICDS), and school meals have contributed to a reduction in absolute poverty as well as previous improvements in nutrition indicators.
- However, there are continuous attempts to weaken these mechanisms through underfunding and general neglect.
- Only about 32.5% of the funds released for Poshan Abhiyaan from 2017-18 onwards had been utilized.
- There are some improvements seen in determinants of malnutrition such as access to sanitation, clean cooking fuels and women’s status – a reduction in spousal violence and greater access of women to bank accounts.
A piecemeal approach
- The overall poor nutritional outcomes show that a piecemeal approach addressing some aspects does not work.
- Direct interventions such as supplementary nutrition (of good quality including eggs, fruits, etc.), growth monitoring, and behaviour change communication through the ICDS and school meals must be strengthened and given more resources.
- Universal maternity entitlements and child care services to enable exclusive breastfeeding, appropriate infant and young child feeding as well as towards recognizing women’s unpaid work burdens have been on the agenda for long, but not much progress has been made on these.
- The linkages between agriculture and nutrition both through what foods are produced and available as well as what kinds of livelihoods are generated in farming are also important.
Conclusion
- The basic determinants of malnutrition – household food security, access to basic health services and equitable gender relations – cannot be ignored any longer.
- An employment-centred growth strategy which includes the universal provision of basic services for education, health, food and social security is imperative.
- There have been many indications in our country that business as usual is not sustainable anymore.
- It is hoped that the experience of the pandemic, as well as the results of NFHS-5, serve as a wake-up call for a serious rethinking of issues related to nutrition and accord these issues priority.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Matru Sahyogini Samitis Scheme
From UPSC perspective, the following things are important :
Prelims level: ICDS, Matru Sahyogini Samitis Scheme
Mains level: Not Much
The MP government has issued an order for the appointment of committees led by mothers to ensure better monitoring of services delivered at Anganwadi or day-care centres across the State.
Try this PYQ:
Q.Which of the following are the objectives of ‘National Nutrition Mission’?
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Matru Sahyogini Samitis
- Called ‘Matru Sahyogini Samiti’ or Mothers’ Cooperation Committees, these will comprise 10 mothers at each Anganwadi centres.
- They would be representing the concerns of different sets of beneficiaries under the Integrated Child Development Services, or National Nutrition Mission.
- Beneficiaries’ would include children between six months to three years, children between three years and six years, adolescent girls and pregnant women and lactating mothers.
- These mothers will keep a watch on weekly ration distribution to them as well as suggest nutritious and tasteful recipes for meals served to children at the centres.
- The move is being taken as per the mandate of the National Food Security Act, 2013 (NFSA).
Its’ functioning
- The committees will include mothers of beneficiary children as well as be represented by pregnant women and lactating mothers who are enrolled under the scheme.
- The Anganwadi scheme includes a package of six services delivered at the centres, including supplementary nutrition, health services including vaccination, early education, among others.
- The Committees will also include a woman panch, women active in the community and eager to volunteer their support to the scheme, teachers from the local school, and women heads of self-help groups (SHG).
Why such a move?
- This is in a move that is aimed at strengthening community response to the problem of hunger and malnutrition in the State.
- With the help of mothers, we will be able to turn anganwadis into a community health system, a nutrition management centre, and spread awareness against social evils.
- These will turn into a model for local governance as well as allow for greater engagement between communities and the State government.
Back2Basics: Integrated Child Development Services (ICDS)
- The ICDS aims to provide food, preschool education, primary healthcare, immunization, health check-up and referral services to children under 6 years of age and their mothers.
- The scheme was launched in 1975, discontinued in 1978 by the government of Morarji Desai, and then relaunched by the Tenth Five Year Plan.
- The tenth FYP also linked ICDS to Anganwadi centres established mainly in rural areas and staffed with frontline workers.
- The ICDS provide for anganwadis or day-care centres which deliver a package of six services including:
- Immunization
- Supplementary nutrition
- Health checkup
- Referral services
- Pre-school education (Non-Formal)
- Nutrition and Health information
Implementation
- For nutritional purposes, ICDS provides 500 kilocalories (with 12-15 grams of protein) every day to every child below 6 years of age.
- For adolescent girls, it is up to 500-kilo calories with up to 25 grams of protein every day.
- The services of Immunisation, Health Check-up and Referral Services delivered through Public Health Infrastructure under the Ministry of Health and Family Welfare.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Threat of malnutrition to promise of India
From UPSC perspective, the following things are important :
Prelims level: POSHAN Abhiyan
Mains level: Paper 2- Analysing the contribution of POSHAN Abhiyan
POSHAN Abhiyan has completed 1000 days. The article analyses the challenges country face on the nutrition front which has been exacerbated by the Covid-19 induced disruptions.
Severity and impact of malnutrition
- Malnourished children tend to fall short of their real potential — physically as well as mentally.
- That is because malnutrition leaves their bodies weaker and more susceptible to illnesses.
- In 2017, a staggering 68% of 1.04 million deaths of children under five years in India was attributable to malnutrition, reckoned a Lancet study in 2019.
- Without necessary nutrients, their brains do not develop to the fullest.
- Malnutrition places a burden heavy enough for India, to make it a top national priority.
- About half of all children under five years in the country were found to be stunted (too short) or wasted (too thin) for their height, estimated the Comprehensive National Nutrition Survey, carried out by the Ministry of Health and Family Welfare with support of UNICEF three years ago.
POSHAN Abhiyan against the background Covid-19 disruption
- The Prime Minister’s Overarching Scheme for Holistic Nutrition (POSHAN) Abhiyaan in 2018, led to a holistic approach to tackle malnutrition.
- Under it, the government strengthened the delivery of essential nutrition interventions.
- COVID-19 is pushing millions into poverty making them vulnerable to malnutrition and food insecurities.
- Pandemic-prompted lockdowns disrupted essential services — such as supplementary feeding under anganwadi centres, mid-day meals, immunisation, and micro-nutrient supplementation which can exacerbate malnutrition.
- Leaders from academia, civil society, development partners, community advocates and the private sector have come together as part of ‘commitment to action’.
- The ‘commitment to action’ includes commitments around sustained leadership, dedicated finances, multi-sectoral approach and increased uninterrupted coverage of a vulnerable population under programmes enhancing nutrition.
Financial commitments
- India already has some of the world’s biggest early childhood public intervention schemes such as the Integrated Child Development Scheme, the mid-day meal programme, and Public Distribution System.
- India needs to ensure coverage of every single child and mother.
- To ensure this, the country needs to retain its financial commitments for nutrition schemes.
- Economic insecurities often force girls into early marriage, early motherhood, discontinue their schooling, and reduce institutional deliveries, cut access to micronutrient supplements, and nutritious food.
- Accelerating efforts to address these will be needed to stop the regression into the deeper recesses of malnutrition.
Conclusion
It takes time for nutrition interventions to yield dividends, but once those accrue, they can bring transformative generational shifts. Filling in the nutrition gaps will guarantee a level-playing field for all children and strengthen the foundations for the making of a future super-power.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Anganwadi centres
From UPSC perspective, the following things are important :
Prelims level: ICDS program
Mains level: Paper 2- Role of Anganwadi centres in ICDS
The article highlights the role of Anganwadi’s in the effective implementation and service delivery under the ICDS.
Gaps in the utilisation of services by ICDS
- The economic fallout of COVID-19 makes the necessity of quality public welfare services more pressing than ever.
- The Integrated Child Development Services (ICDS) programme is one such scheme.
- ICDS caters to the nutrition, health and pre-education needs of children till six years of age as well as the health and nutrition of women and adolescent girls.
- However, recent reports have shown gaps in the utilisation of services.
Recasting the Anganwadi centres
- Anganwadi centres (AWCs) could become agents of improved delivery of ICDS’s services.
- According to government data, the country has 13.77 lakh Anganwadi centres (AWCs).
- These centres have expanded their reach, but they need to play a much larger role in anchoring community development.
- Nearly a fourth of the operational AWCs lack drinking water facilities and 36 per cent do not have toilets.
- In 2015, the NITI Aayog recommended better sanitation and drinking water facilities, improved power supply and basic medicines for the AWCs.
- NITI Aayog also suggested that these centres be provided with the required number of workers, whose skills should be upgraded through regular training.
- It has acknowledged the need to improve anganwadi centres.
- The Central government’s Saksham Anganwadi Scheme aims to upgrade 2.5 lakh such centres across the country. It is up to the state governments to take up the baton
- Only a limited number of AWCs have facilities like creche, and good quality recreational and learning facilities for pre-school education.
- An approach that combines an effective supplementary nutrition programme with pedagogic processes that make learning interesting is the need of the hour.
Steps taken for effective implementation of ICDS
- Effective implementation of the ICDS programme rests heavily on the combined efforts of the anganwadi workers (AWWs), ASHAs and ANMs.
- The Centre’s POSHAN Abhiyaan has taken important steps towards building capacities of AWWs.
- Technology can also be used for augmenting the programme’s quality.
- AWWs have been provided with smartphones and their supervisors with tablets, under the government schemes.
- Apps on these devices track the distribution of take-home rations and supplementary nutrition services.
- The data generated should inform decisions to improve the programme.
- In Andhra Pradesh and Telangana, anganwadi centres have been geotagged to improve service delivery.
- Gujarat has digitised the supply chain of take-home rations and real-time data is being used to minimise stockouts at the anganwadi centres.
Conclusion
Government must act on the three imperatives. First, while infrastructure development and capacity building of the anganwadi remains the key to improving the programme, the standards of all its services need to be upscaled. Second, states have much to learn from each other’s experiences. Third, anganwadi centres must cater to the needs of the community and the programme’s workers.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[pib] Thalassemia Bal Sewa Yojna
From UPSC perspective, the following things are important :
Prelims level: Thalassemia
Mains level: Not Much
Union Health Ministry has launched the second phase of “Thalassemia Bal Sewa Yojna” for underprivileged Thalassemic patients.
Thalassemia Bal Sewa Yojna
- This scheme was launched in 2017 under the Coal India CSR funded Hematopoietic Stem Cell Transplantation (HSCT) program.
- It aims to provide a one-time cure opportunity for Haemoglobinopathies like Thalassaemia and Sickle Cell Disease for patients who have a matched family donor.
- The initiative was targeted to provide financial assistance to a total of 200 patients by providing a package cost not exceeding Rs. 10 lakhs per HSCT.
What is Thalassemia?
- Thalassemia is an inherited blood disorder characterized by less oxygen-carrying protein (haemoglobin) and fewer red blood cells in the body than normal.
- When there isn’t enough haemoglobin, the body’s red blood cells don’t function properly and they last shorter periods of time, so there are fewer healthy red blood cells travelling in the bloodstream.
- Symptoms include fatigue, weakness, paleness and slow growth.
- Mild forms may not need treatment. Severe forms may require blood transfusions or a donor stem-cell transplant.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Assisted Reproductive Technology Bill needs a thorough review
From UPSC perspective, the following things are important :
Prelims level: ART Bill
Mains level: Paper 2- Concerns with the ART Bill
There are several issues with the Assisted Reproductive Technology Bill and these issues need consideration before the passage of the Bill.
What the Bill aims to achieve
- Union Health Minister introduced the Assisted Reproductive Technology (Regulation) Bill, 2020 (Bill) in the Lok Sabha.
- Its aim is to regulate ART banks and clinics, allow safe and ethical practice of ARTs and protect women and children from exploitation.
- The Bill was introduced to supplement the Surrogacy (Regulation) Bill, 2019 (SRB), which awaits consideration by the Rajya Sabha after review by two parliamentary committees.
Concerns with the Bill
1) Exclusion in the access of ART
- .The Bill allows for a married heterosexual couple and a woman above the age of marriage to use ARTs.
- It excludes single men, cohabiting heterosexual couples and LGBTQI individuals and couples from accessing ARTs.
- This violates Article 14 of the Constitution and the right to privacy jurisprudence of Puttaswamy, where the Supreme Court held that “ the liberty of procreation, the choice of a family life” concerned all individuals irrespective of their social status and were aspects of privacy.
- In Navtej Johar case, Justice Chandrachud exhorted the state to take positive steps for equal protection for same-sex couples.
- Unlike the SRB, there is no prohibition on foreign citizens accessing ARTs.
- Foreigners can access ART but not Indian citizens in loving relationships.
- This fails to reflect the true spirit of the Constitution.
2) Consent
- The ART Bill does little to protect the egg donor.
- Harvesting of eggs is an invasive process which, if performed incorrectly, can result in death.
- The Bill requires an egg donor’s written consent but does not provide for her counselling or the ability to withdraw her consent before or during the procedure.
- She receives no compensation or reimbursement of expenses for loss of salary, time and effort.
- Failing to pay for bodily services constitutes unfree labour, which is prohibited by Article 23 of the Constitution.
- The commissioning parties only need to obtain an insurance policy in her name for medical complications or death; no amount or duration is specified.
- The egg donor’s interests are subordinated in a Bill proposed in her name.
- The Bill restricts egg donation to a married woman with a child (at least three years old).
3) Threat of eugenics
- The Bill requires pre-implantation genetic testing.
- If the embryo suffers from “pre-existing, heritable, life-threatening or genetic diseases”, it can be donated for research with the commissioning parties’ permission.
- These disorders need specification or the Bill risks promoting an impermissible programme of eugenics.
4) Overlap with Surrogacy Regulation
- There is considerable overlap between ART and SRB sectors. Yet the Bills do not work in tandem.
- Core ART processes are left undefined; several of these are defined in the SRB.
- Definitions of commissioning “couple”, “infertility”, “ART clinics” and “banks” need to be synchronised between the Bills.
- A single woman cannot commission surrogacy but can access ART.
- The Bill designates surrogacy boards under the SRB to function as advisory bodies for ART, which is desirable.
- However, both Bills set up multiple bodies for registration which will result in duplication or lack of regulation (e.g. surrogacy clinic is not required to report surrogacy to National Registry).
- Also, the same offending behaviours under both Bills are punished differently + punishments under the SRB are greater.
- Offences under the Bill are bailable but not under the SRB.
- Finally, records have to be maintained for 10 years under the Bill but for 25 years under the SRB.
- The same actions taken by a surrogacy clinic and ART clinic attract varied regulation.
Other concerns
- Children born from ART do not have the right to know their parentage, which is crucial to their best interests and protected under previous drafts.
- There is no distinction between ART banks and ART clinics, given that gamete donation is not compensated, economically viability of ART Banks raises a question.
- In previous drafts, gametes could not be gifted between known friends and relatives if this is not changed, gamete shortage is likely.
- The Bill’s prohibition on the sale, transfer, or use of gametes and embryos is poorly worded and will confuse foreign and domestic parents relying on donated gametes.
- Unusually, the Bill requires all bodies to be bound by the directions of central and state governments in the national interest, friendly relations with foreign states, public order, decency or morality — being broadly phrased, it undermines their independence.
Way forward
- The Bill to maintain a grievance cell but clinics must instead have ethics committees.
- Mandated counselling services should also be independent of the clinic.
- The poor enforcement of the PCPNDT Act, 1994, demonstrates that enhanced punishments do not secure compliance — lawyers and judges also lack medical expertise.
- Patients already sue fertility clinics in consumer redressal fora, which is preferable to criminal courts.
Conclusion
The Bill raises several constitutional, medico-legal, ethical and regulatory concerns, affecting millions and must be thoroughly reviewed before passage.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Making malnutrition free India by 2030
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2- Malnutrition and health of the child
The article analyses the problem of malnutrition in India and suggests the pathways to achieve the malnutrition free India by 2030.
Severity of the nourishment problem in India
- There were 189.2 million undernourished people (28 per cent of the world) in India in 2017-19, as per the combined report of FAO, IFAD, UNICEF, WFP and WHO (FAO, et.al. 2020) on “The state of Food Security and Nutrition in the World”.
- India accounts for 28 per cent (40.3 million) of the world’s stunted children (low height-for-age) under five years of age, and 43 per cent (20.1 million) of the world’s wasted children (low weight-for-height) in 2019.
- In India, the problem has been more severe amongst children below the age of five years.
- As per the National Family Health Survey (NFHS, 2015-16), the proportion of underweight and stunted children was as high as 35.8 per cent and 38.4 per cent respectively.
- In several districts of Bihar, Jharkhand, Uttar Pradesh, Madhya Pradesh, Rajasthan and even Gujarat, the proportion of underweight children was more than 40 per cent.
Aims of the National Nutrition Mission (NNM)
- Ending all forms of malnutrition by 2030 is also the target of Sustainable Development Goal (SDG-2) of Zero Hunger.
- Towards this end, NNM aims to reduce stunting, underweight and low birth weight each by 2 per cent per annum.
- It aims to reduce anaemia among children, adolescent girls and women, each by 3 per cent per annum by 2022.
- However, the Global Burden of Disease Study 1990–2017 has estimated that if the current trend continues, India cannot achieve these targets under NNM by 2022.
Understanding the key determinants and deciding policy response
1) Mothers’ education
- Mothers’ education, particularly higher education, has the strongest inverse association with under-nutrition.
- Women’s education has a multiplier effect not only on household food security but also on the child’s feeding practice and the sanitation facility.
- Despite India’s considerable improvement in female literacy, only 13.7 per cent of women have received higher education (NFHS, 2015-16).
- Therefore, programmes that promote women’s higher education such as liberal scholarships for women need to be accorded a much higher priority.
2) Sanitation and access to safe drinking water
- The second key determinant of child under-nutrition is the wealth index, which subsumes access to sanitation facilities and safe drinking water.
- WASH initiatives, that is, safe drinking water, sanitation and hygiene, are critical for improving child nutritional outcomes.
- In this context, the Swachh Bharat Abhiyan aims to eliminate open defecation and bring about behavioural changes in hygiene and sanitation practices.
- In five years of the Abhiyan, as per government records, rural sanitation coverage has gone from 38.7 per cent in 2014 to 100 per cent in 2019, while the sanitation coverage in urban cites has gone up to 99 per cent by September 2020.
- This remarkable achievement of the Swachh Bharat Abhiyan, subject to third-party evaluations, is expected to have a multiplier effect on nutritional outcomes.
3) Leveraging agricultural policies
- We should leverage agricultural policies and programmes to be more “nutrition-sensitive” and reinforcing diet diversification towards a nutrient-rich diet.
- Food-based safety nets in India are biased in favour of staples: rice and wheat.
- They need to provide a more diversified food basket, including coarse grains, millets, pulses and bio-fortified staples.
- Bio-fortification is very cost-effective in improving the diet of households and the nutritional status of children.
- The Harvest-Plus programme of CGIAR can work with the Indian Council of Agricultural Research (ICAR) to grow new varieties of nutrient-rich staple food crops.
4) Promotion of exclusive breastfeeding, complementary foods, diversified diet
- The promotion of exclusive breastfeeding and the introduction of complementary foods and a diversified diet after the first six months is essential to meet the nutritional needs of infants and ensure appropriate growth and cognitive development of children.
5) Access to prenatal and postnatal care
- Access and utilisation of prenatal and postnatal health care services also play a significant role in curbing undernutrition among children.
- Aanganwadi workers and community participation can bring significant improvements in child-caring practices.
Consider the question “Assess the severity the problem of malnutrition in India and suggest the measure to achieve the goal of malnutrition free India by 2030”
Conclusion
To contribute towards the holistic nourishment of children and a malnutrition free India by 2030, the government needs to address the multi-dimensional determinants of malnutrition on an urgent basis.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Increasing age of marriage will be exercise of carceral power by state
From UPSC perspective, the following things are important :
Mains level: Paper 2-Increasing the age of marriage for girls and implications
The article examines the issue of the age of marriage of girls and its relation with their education level and economic status.
Trends in early marriage
- The National Family Health Survey (NFHS-4) data 2015-16 points to certain trends in early marriages:
- That rural women are likely to marry earlier than their urban counterparts.
- The higher up a woman is on the wealth quintile, the later she marries.
- Most importantly, it establishes a direct causal link between education levels and delayed age of marriage.
- Women with 12 years or more of schooling are most likely to marry later.
- Only 8 per cent rural girls who drop out in the age group 6 to 17 years cite marriage as the reason.
Impact on STs and SCs
- According to the wealth quintile data, the poorest households are concentrated in rural India.
- The lowest quintile, which is most likely to marry off their girls early out of socio-economic necessities, have 45 per cent of the Scheduled Tribe (ST) and 25.9 per cent Scheduled castes.
- The NFHS-4 data on women aged 15-49 by number of years of schooling completed shows that 42 per cent ST women and 33 per cent SC women have received no schooling.
Issues
- Marriages in India are governed by various personal laws which set varying minimum ages for girls as also the Prohibition of Child Marriage Act (PCMA), 2006, where it is 18 years for girls and 21 for boys.
- This is compounded by The Protection of Children from Sexual Offences (POCSO) Act, 2012, that increased the age of consent, from 16 years to 18 years.
- Several studies have shown how this has criminalised self-arranged adolescent marriages as parents often misuse it to punish couples marrying without their approval, especially in cases of inter-caste marriages.
Way forward
- The National Human Rights Commission showed how higher education levels lead to a lower likelihood of women being married early and recommended that the Right to Education Act, 2009, be amended to make it applicable up to the age of 18 years.
- Noting the law’s patriarchal underpinnings, the 18th Law Commission report (2008) asked for uniformity in the age of marriage at 18 years for both men and women and lowering the age of consent to 16 years. Government could act on such a recommendation.
Consider the question “What are the advantages of increasing the minimum age of marriage for girls. Also, examine the issues with the move.
Conclusion
The median age at first marriage for both men and women in India has registered a significant decadal improvement with more people now marrying later than ever before. Any attempt to leapfrog through quick-fix and ill-conceived punitive measures will only considerably reverse these gains.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Increasing the age of marriage for girls and related issues
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2- Increasing the age of marriage for girls
The article analyses the issues with objectives of increasing the age of marriage for girls.
Poverty of mother: Important factor
- Raising the age of marriage is the could be the way to improve the health and nutritional status of mothers and their infants.
- An article published in the journal The Lancet Child and Adolescent Health analyses data on stunting in children and thinness in mothers in the latest round of the National Family Health Survey 4 (2015-16).
- The authors examine the strength of the association between many different causal factors.
- As it turns out, the poverty of the mother plays the greatest role of all by far.
- Instead of early pregnancy causing malnourishment, they may both be the consequences of poverty.
- The best way to go about breaking such a cycle would be to pick the factors perpetuating it, it would be the poverty of the mother in this case.
Declining fertility rate in India
- India’s fertility rates have been declining to well below replacement levels in many States, including those with higher levels of child marriage.
- This could be the reason for the shift from fuelling fears about booming populations to expressing concern for the undernourishment of children.
- So, the problem of “populations explosion” is not the real problem as the demographic data suggests.
Concern
- The change in the marriage age will leave the vast majority of Indian women who marry before they are 21 without the legal protections.
Conclusion
The proposal and the objective to be achieved through raising the age of marriage needs reconsideration for the reasons cited above.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
PCPNDT Act and rule changes during pandemic
From UPSC perspective, the following things are important :
Prelims level: Not much
Mains level: Paper 2-PCPNDT Act
The article deals with the issues of suspension of some requirements under PCPNDT Act. It also discusses the role judiciary played in 25-years jurisprudence around the Act.
Context
- Last week, the Supreme Court deferred a pronouncement on the legality of the Centre’s now-lapsed controversial notification relating to the rules of the law banning sex-selective abortions.
- The apex court similarly erred on the side of caution in June, choosing not to stay the Ministry of Health and Family Welfare’s gazette notification.
What were the changes
- One of the rules requires a five-yearly renewal of registration of genetic laboratories, ultrasound clinics and imaging centres, subject to the fulfilment of eligibility criteria.
- Another mandate to submit monthly records on the conduct of pregnancy-related procedures to the designated authority.
- State governments and Union Territories are required to furnish quarterly reports to the Centre on the implementation of the law.
- The Union Health Ministry had maintained that various procedural deadlines were relaxed in the wake of the public health crisis and that such flexibility would in no way jeopardise the larger objectives of the law.
Issues with the suspension
- Activists saw no rationale behind the suspension of rules, since the operation of diagnostic laboratories had been declared essential services.
- They were understandably apprehensive that the freeze would result in large-scale violations.
- It is one thing to offer relaxation for delays in the completion of formalities via an administrative order, but altogether another to declare a freeze via a gazette notification, they argued.
Court judgements on PCPNDT Act
- The 25-year jurisprudence around the PCPNDT legislation does not justify a casual approach on the enforcement of its various provisions.
- The Court last year ruled that the non-maintenance of medical records as per Section 23 of the PCPNDT Act could serve as a conduit in the grave offence of foeticide.
- In its 2016 judgment, the Supreme Court authorised the seizure of illegal equipment from clinics and the suspension of their registration as well as speedy disposal of relevant cases by the States.
Consider the question “How far has the PCPNDT Act been successful in dealing with the menace of sex-selective abortion? What are the shortcomings in the Act?”
Conclusion
Crucially, the alarming decline witnessed in recent decades in India’s sex ratio at birth calls for uncompromising adherence to public policy, more than is evident from evolving case law.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Seeking a more progressive abortion law
From UPSC perspective, the following things are important :
Prelims level: Not much.
Mains level: Paper 2- Shortcomings in the Medical Termination of Pregnancy Act 1971 and need of the more progressive abortion law in the country.
Context
The Medical Termination of Pregnancy Bill doesn’t do enough to secure women’s choices and interests.
Deaths due to unsafe abortion and previous attempts to legislate
- Deaths due to unsafe abortions: Recent reports have shown that more than 10 women die every day due to unsafe abortions in India.
- And backward abortion laws only contribute to women seeking illegal and unsafe options.
- The Cabinet has recently approved the Medical Termination of Pregnancy (Amendment) Bill, 2020 (MTP Bill, 2020) which will soon be tabled in Parliament.
- It seeks to amend the Medical Termination of Pregnancy Act, 1971 (MTP Act) and follows the MTP Bills of 2014, 2017 and 2018, all of which previously lapsed in Parliament.
Provisions of the current law
- Foetus-age based division: The MTP Act divides its regulatory framework for allowing abortions into categories, according to the gestational age of the foetus.
- Up to 12 weeks: Under Section 3, for foetuses that are aged up to 12 weeks-
- Only one medical practitioner’s opinion is required to the effect that the continuance of the pregnancy would pose a risk to the life of the mother or cause grave injury to her physical or mental health.
- Or there is a substantial risk that if the child is born, it would suffer from such physical or mental abnormalities as to be seriously handicapped.
- Between 12 weeks and 20 weeks: But if the foetus is aged between 12 weeks and 20 weeks-
- At least two medical practitioners’ opinions conforming to either of the two conditions are required.
- What beyond 20 weeks? Beyond 20 weeks, termination may be carried out where it is necessary to save the life of the pregnant woman.
- Definition of grave injury: The MTP Act also specifies that ‘grave injury’ may be explained as
- The anguish caused by a pregnancy arising out of rape, or the anguish caused by an unwanted pregnancy arising out of the failure of a contraceptive used by a married woman or her husband.
What are the issues with the current law?
- Several issues arise from the current framework under the MTP Act.
- First-Lac of autonomy of women: At all stages of the pregnancy, the healthcare providers, rather than the women seeking an abortion, have the final say on whether the abortion can be carried out.
- It is true that factors such as failure of contraceptives or grave injury are not required to be proved under the MTP Act.
- However, to get the pregnancy terminated solely based on her will, the woman may be compelled to lie or plead with the doctor.
- Thus, at present, pregnant women lack autonomy in making the decision to terminate their pregnancy and have to bear additional mental stress, as well as the financial burden of getting a doctor’s approval.
- On request abortion in 67 countries: Indian’s law is unlike the abortion laws in 67 countries, including Iceland, France, Canada, South Africa and Uruguay, where a woman can get an abortion ‘on request’ with or without a specific gestational limit (which is usually 12 weeks).
- Second-Prejudice against unmarried women: The MTP Act embodies a clear prejudice against unmarried women.
- According to ‘Explanation 2’ provided under Section 3(2) of the Act, where a pregnancy occurs due to failure of any birth control device or method used by any “married woman or her husband”, the anguish caused is presumed to constitute a “grave injury” to the mental health of the pregnant woman.
- While the applicability of this provision to unmarried women is contested, there is always the danger of a more restrictive interpretation, especially when the final decision rests with the doctor and not the woman herself.
- Third-Restriction of 20 weeks’ limit: Due to advancements in science, foetal abnormalities can now be detected even after 20 weeks.
- Danger to mother’s life only condition after 20 weeks: The MTP Act presently allows abortion post 20 weeks only where it is necessary to save the life of the mother.
- Problem with this restriction: The above restriction means that even if a substantial foetal abnormality is detected and the mother doesn’t want to bear life-long caregiving responsibilities and the mental agony associated with it, the law gives her no recourse unless there is a prospect of her death.
What does the bill fail to address?
- While the MTP Bill, 2020, is a step in the right direction, it still fails to address most of the problems with the MTP
- First, it doesn’t allow abortion on request at any point after the pregnancy.
- Second, it doesn’t take a step towards removing the prejudice against unmarried women by amending the relevant provision.
- And finally, it enhances the gestational limit for legal abortion from 20 to 24 weeks only for specific categories of women such as survivors of rape, victims of incest, and minors.
- This means that a woman who does not fall into these categories would not be able to seek an abortion beyond 20 weeks, even if she suffers from a grave physical or mental injury due to the pregnancy.
What are the provisions for the case of foetal abnormality in the bill?
- Limit irrelevant if the foetal abnormality is diagnosed by the Medical Board: The Bill does make the upper gestational limit irrelevant in procuring an abortion if there are substantial foetal abnormalities diagnosed by the Medical Board.
- This means that even if there is no threat to the mother’s life, she would be able to procure an abortion as soon as a substantial foetal abnormality comes to light.
- While this is an important step and would have in the past helped many women who fought long battles in Court without recourse.
- Rules against unnecessary delays: It is crucial that this provision is accompanied by appropriate rules for the Medical Boards that guard against unnecessary delays, which only increase the risks associated with a late abortion.
Conclusion
- Recognition of women’s right: The Supreme Court has recognised women’s right to make reproductive choices and their decision to abort as a dimension of their personal liberty (in X v. Union of India,2017) and as falling within the realm of the fundamental right to privacy (in K.S. Puttaswamy v. Union of India, 2017). Yet, current abortion laws fail to allow the exercise of this right.
- The bill does not do enough: While it is hoped that MTP Bill, 2020 will not lapse in Parliament like its predecessors, it is evident that it does not do enough to secure women’s interests, and there is still a long road ahead for progressive abortion laws.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[op-ed of the day] Amendments to Medical Termination of Pregnancy Act are a mixed bag
From UPSC perspective, the following things are important :
Prelims level: Not much.
Mains level: Paper 2- Medical Termination of Pregnancy Act amendment and issues involved.
Context
The Union Cabinet’s approval of the amended Medical Termination of Pregnancy (MTP) Bill 2020 was reported on January 29. This amendment was long due and has made some anticipated changes demanded by women’s groups and courts, including the Supreme Court.
Why the amendment was necessitated?
- Abortion (unsafe) accounts for almost 10 per cent of maternal deaths in India.
- No provision to avoid unsafe abortion: The amended Act doesn’t have any new substantial provisions to avoid unsafe abortions.
- The right to safe abortion (at least till 12 weeks, when it is safer) would have made the state responsible to provide safe abortion services.
- Reduce the burden on judiciary: The proposed amendments will definitely reduce the burden on the judiciary, especially given the plethora of cases seeking permission for abortion beyond the prescribed duration of 20 weeks.
- Two types of Court cases: The court cases are broadly two types.
- The first group of cases: These are pregnancies that extend beyond 20 weeks of gestation as a result of rape, incest or of minor women.
- The new Act rightly addresses these by extending prescribed period abortion to 24 weeks.
- However, such cases form a minuscule proportion of the total number. For such cases, even the 24-week cap can be done away with, provided the abortions can be safely done.
- The second group of cases
- These are of pregnancies that become unwanted after congenital foetal anomalies are found upon testing.
- With advancements in prenatal foetal screening/diagnostic technologies, more such cases are knocking at the doors of courts.
- Marginal interval under the current act: Anomalies detected at 17-20 weeks provide only a marginal interval to conduct an abortion under the current Act.
- The extension to 24 weeks seems to give cover to these cases for abortion services, reducing the burden on courts.
How the law could be misused?
- Possibility of using any anomaly as a ground for abortion: The amendments have opened up the possibility for any congenital anomaly to be used as grounds for abortion.
- Anomalies which are incompatible with life provide grounds for access to abortion at any time during pregnancy -not just 24 weeks of gestation-as long as the woman desires it and it doesn’t endanger her health.
- But with advancements in diagnostic technologies, more anomalies will be detected, including those which are compatible with life.
- Social acceptability and anomaly: What constitutes an anomaly changes depending on what is considered socially desirable.
- Issue of raising children with disability: Technology-aided detection of “undesirability” could now find social support, as has been the case with female foetuses.
- This raises concerns that raising children with disability, especially in the absence of state support and poor social attitudes, could go down a similar path.
The risk to the life of women
- Abortion beyond 12 weeks carries serious health risks.
- 12 weeks provision under current law: Current law requires the expert opinion of two registered medical practitioners for the abortion beyond 12 weeks.
- Extending the limit to 20 weeks and risk involved: 12-week requirement has been delayed till 20 weeks, though the physiology of pregnancy and risks associated with procedures for second-trimester abortions haven’t changed significantly.
- Possibility of more complications: Without the strengthening of public services, easing second-trimester abortions between 12-20 weeks opens the possibilities of more complications and endangers the life of the woman.
- 12 weeks provision under current law: Current law requires the expert opinion of two registered medical practitioners for the abortion beyond 12 weeks.
Conclusion
With congenital anomalies as a ground for abortion, the eugenic mindset of having socially desirable children could push more women into risky late abortions. The approach of medical boards advising courts in cases of late abortions under this Act will be critical to balancing women’s right to choose with risk to the woman and the motives for abortion. The rules framed under the Act must address this in no uncertain terms.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[pib] The Medical Termination of Pregnancy (Amendment) Bill, 2020
From UPSC perspective, the following things are important :
Prelims level: Highlights of the bill
Mains level: MTP: Ethical and health issues surrounding it
The Union Cabinet has approved the Medical Termination of Pregnancy (Amendment) Bill, 2020 to amend the Medical Termination of Pregnancy Act, 1971.
About the Bill
- The Medical Termination of Pregnancy (Amendment) Bill, 2020 is for expanding access of women to safe and legal abortion services on therapeutic, eugenic, humanitarian or social grounds.
- It aims to increase upper gestation limit for termination of pregnancy under certain conditions and to strengthen access to comprehensive abortion care, under strict conditions, without compromising service and quality of safe abortion.
Salient features of proposed amendments:
- Proposing requirement for opinion of one provider for termination of pregnancy, up to 20 weeks of gestation and introducing the requirement of opinion of two providers for termination of pregnancy of 20-24 weeks of gestation.
- Enhancing the upper gestation limit from 20 to 24 weeks for special categories of women which will be defined in the amendments to the MTP Rules and would include ‘vulnerable women including survivors of rape, victims of incest and other vulnerable women (like differently-abled women, Minors) etc.
- Upper gestation limit not to apply in cases of substantial foetal abnormalities diagnosed by Medical Board. The composition, functions and other details of Medical Board to be prescribed subsequently in Rules under the Act.
- Anonymity of the person: Name and other particulars of a woman whose pregnancy has been terminated shall not be revealed except to a person authorised in any law for the time being in force.
Benefits
- It is a step towards safety and well-being of the women and many women will be benefitted by this.
- Recently several petitions were received by the Courts seeking permission for aborting pregnancies at a gestational age beyond the present permissible limit on grounds of foetal abnormalities or pregnancies due to sexual violence faced by women.
- The proposed increase in gestational age will ensure dignity, autonomy, confidentiality and justice for women who need to terminate pregnancy.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
ICDS Programme
From UPSC perspective, the following things are important :
Prelims level: ICDS and its components
Mains level: Forms of malnutrition in urban areas and their preventive measures

Centre seeks to revamp the ICDS scheme in urban areas. For this NITI Aayog will develop draft policy, which will be circulated to the Ministries for consultations.
Integrated Child Development Services (ICDS)
- The ICDS is a government programme in India which provides food, preschool education, primary healthcare, immunization, health check-up and referral services to children under 6 years of age and their mothers.
- The scheme was launched in 1975, discontinued in 1978 by the government of Morarji Desai, and then relaunched by the Tenth Five Year Plan.
- Tenth FYP also linked ICDS to Anganwadi centres established mainly in rural areas and staffed with frontline workers.
- The ICDS provide for anganwadis or day-care centres which deliver a package of six services including:
- Immunization
- Supplementary nutrition
- Health checkup
- Referral services
- Pre-school education(Non-Formal)
- Nutrition and Health information
Implementation
- For nutritional purposes ICDS provides 500 kilocalories (with 12-15 grams of protein) every day to every child below 6 years of age.
- For adolescent girls it is up to 500 kilo calories with up to 25 grams of protein every day.
- The services of Immunisation, Health Check-up and Referral Services delivered through Public Health Infrastructure under the Ministry of Health and Family Welfare.
Revamp for Urban Areas
- Health and ICDS models that work in rural areas may not work in urban areas because of higher population density, transportation challenges and migration.
- Children in urban areas were overweight and obese as indicated by subscapular skinfold thickness (SSFT) for their age.
- The first-ever pan-India survey on the nutrition status of children, highlighted that malnutrition among children in urban India.
- It found a higher prevalence of obesity because of relative prosperity and lifestyle patterns, along with iron and Vitamin D deficiency.
- According to government data from 2018, of the 14 lakh anganwadis across the country there are only 1.38 lakh anganwadis in urban areas.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
Pulse Polio Programme
From UPSC perspective, the following things are important :
Prelims level: Polio and its vaccine
Mains level: Pulse Polio Programme
The beginning of this year’s Pulse Polio Programme was inaugurated from the Rashtrapati Bhavan itself. To prevent the virus from coming to India, the government has since March 2014 made the Oral Polio Vaccination (OPV) mandatory for those travelling between India and polio-affected countries.
The Pulse Polio Programme
- India launched the Pulse Polio immunisation programme in 1995, after a resolution for a global initiative of polio eradication was adopted by the World Health Assembly (WHA) in 1988.
- Children in the age group of 0-5 years are administered polio drops during national and sub-national immunisation rounds (in high-risk areas) every year.
India is polio-free
- According to the Ministry of Health, the last polio case in the country was reported from Howrah district of West Bengal in January 2011.
- The WHO on February 24, 2012, removed India from the list of countries with active endemic wild polio virus transmission.
- Two years later, the South-East Asia Region of the WHO, of which India is a part, was certified as polio-free.
Back2Basics
What is Polio?
- The WHO defines polio or poliomyelitis as a highly infectious viral disease, which mainly affects young children.
- The virus is transmitted by person-to-person, spread mainly through the faecal-oral route or, less frequently, by a common vehicle (e.g. contaminated water or food) and multiplies in the intestine, from where it can invade the nervous system and can cause paralysis.
- Initial symptoms of polio include fever, fatigue, headache, vomiting, stiffness in the neck, and pain in the limbs. In a small proportion of cases, the disease causes paralysis, which is often permanent.
- There is no cure for polio, it can only be prevented by immunization.
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
Mother and Child Health – Immunization Program, BPBB, PMJSY, PMMSY, etc.
[op-ed snap] Children of lesser gods
From UPSC perspective, the following things are important :
Prelims level: Not much.
Mains level: Paper 2- Health.
Context
The deaths of nearly 200 children in Kota, from largely preventable diseases, lays bare the condition of the healthcare system in India.
Where does India stand?
- According to UNICEF’s ‘State of World’s Children 2019’ report, India reported the maximum number of deaths of children under five in the world in 2018.
- 8,82,000 children under five died that year.
- That means around 2,416 deaths per day.
- The death of children due to largely-preventable illnesses is a matter of serious concern and calls for urgent introspection.
Factors that govern child health
- Most of the children who died in Gorakhpur, Muzaffarpur and Kota belong to the lowest strata of the society.
- It won’t be wrong to conclude that they were victims of structural violence.
- This structural violence is unleashed through a multitude of social, political and economic factors apathy of healthcare professionals, poor health services/infrastructure
- And low rates of female literacy, economic inequality, the rigid caste system, social apartheid, lack of political will and patriarchy play role.
- As a society, we have stopped looking at the deaths of our citizens through the prism of compassion and concern.
- Structural violence influences the nature and distribution of extreme suffering.
What is being done in the wrong way?
- The government is considering the takeover of 750 district hospitals by private medical colleges through a public-private partnership (PPP) model.
- This, despite ample evidence about the failure of the model in the country’s healthcare system.
- Nobel laureate Kenneth Arrow demonstrated that profit and private involvement in healthcare lead to an erosion of trust.
- An Individual’s demand for medical services is irregular and unpredictable, the involvement of a private market model for such services can be disastrous.
- The U.S.’s experiences in the PPP model in healthcare have shone a light on the deficits in transparency and highlighted the lack of care of vulnerable groups.
Conclusion
- What urgently a sincere engagement by the state in matters concerning peoples’ health.
- We need to question the government’s priorities in a country where nearly a million children die every year
Get an IAS/IPS ranker as your 1: 1 personal mentor for UPSC 2024
- Aim: To generate awareness and improve efficiency of delivery of welfare services meant for women
- Launched on 22 January 2015 with an initial corpus of Rs. 100 crore
- Joint initiative of Ministries of Women & Child Development, Health & Human Resource Development
Districts Identified
The three criteria for selection of districts:
- Districts below the national average (87 districts/23 states);
- Districts above national average but shown declining trend (8 districts/8 states)
- Districts above national average and shown increasing trend (5 districts/5 states- selected so that these CSR levels can be maintained and other districts can emulate and learn from their experiences)
- First Phase:
100 districts have been identified on the basis of low Child Sex Ratio as per Census 2011 covering all States/UTs as a pilot With at least one district in each state
- Second Phase
The scheme has further been expanded to 61 additional districts selected from 11 States/UT having CSR below 918
Strategies:
- Implement a sustained Social Mobilization and Communication Campaign to create equal value for the girl child & promote her education
- Focus on Gender Critical Districts and Cities low on CSR for intensive & integrated action
- Mobilize & Train Panchayati Raj Institutions/ Urban local bodies/ Grassroot workers as catalysts for social change
- Ensure service delivery structures/ schemes & programmes are sufficiently responsive to issues Of gender and children’s rights
- Enable Inter-sectoral and inter-institutional convergence at District/ Block/ Grassroot levels
Implementation:
- Centre: A National Task Force (NTF) headed by Secretary WCD
State: A State Task Force (STF) - District: District Task Force (DTF) headed by the District Collector/ Deputy Commissioner with representation of concerned departments
- Block: A Block Level Committee headed by SDM/ SDO/ BDO
- Gram Panchayat/ Municipality: Respective Panchayat Samiti/ Ward Samiti
- Village: Village Health Sanitation and Nutrition Committees
Published with inputs from Swapnil